Quick Navigation
Let's talk about underbites. You know, that thing where your lower jaw sticks out further than your upper one. Maybe you've lived with it your whole life, or maybe you're noticing it in your kid's smile. It's more than just a cosmetic thing – though let's be honest, that part bugs a lot of people – it's a functional puzzle that can affect how you eat, speak, and even breathe.
I remember chatting with a friend who had a pretty noticeable underbite. He hated getting his picture taken from the side. "I look like a bulldog," he'd joke, but you could tell it wasn't really funny to him. He had no idea it could be causing his constant jaw aches and headaches. That's the thing about an underbite; it's easy to write it off as just how your face is built, but sometimes it's asking for help.
So what's really going on in there? Is it just genetics, or is there more to the story? And more importantly, what can you actually do about it? Braces? Surgery? Some newfangled appliance? The information out there is a mess – some sites make it sound terrifying, others oversimplify it. I dug through the research and talked to experts to cut through the noise.
What's Really Causing That Underbite?
It's rarely just one thing. Think of it like a recipe gone slightly wrong. You need the right amounts of jawbone, teeth, and muscle, all cooked at the right time during growth.
The big player is usually genetics. If your parents or grandparents had a prominent jaw, chances are higher you might inherit the blueprint. Certain genetic syndromes, like Crouzon syndrome or basal cell nevus syndrome, list underbite as a common feature, but these are much rarer. For most people, it's just the family jawline making a strong appearance.
But your genes aren't the whole story. Childhood habits can nudge development in the wrong direction. Thumb sucking, prolonged pacifier use, or tongue thrusting (pushing your tongue against your teeth when you swallow) can apply constant pressure. Over years, that pressure can encourage the lower jaw to grow forward or the upper jaw to grow less than it should. It's like a slow, steady push on a growing tree branch.
Then there's the simple mismatch. Sometimes the upper jaw is underdeveloped (too small or set back). Sometimes the lower jaw is overdeveloped (too large or too far forward). Often, it's a combination of both. An injury to the jaw joints or face during childhood can also throw a wrench in the normal growth process.
It's Not Just About Looks: The Real Impact of an Underbite
Okay, so your bite is off. Big deal, right? Well, your teeth and jaws are a system, and when one part is out of alignment, it puts stress on the whole system.
First, let's talk wear and tear. With an underbite, your teeth don't meet the way they're designed to. The front teeth, which are meant for biting, end up grinding against each other. This can lead to excessive enamel wear, chipping, and even fractures. I've seen cases where the edges of the front teeth were worn flat from years of this abnormal contact. Not good.
Then there's the jaw joint – the temporomandibular joint (TMJ). This hinge is a precision instrument. An underbite forces it into an unnatural position to get your teeth to meet. The result? A higher risk of temporomandibular joint disorder (TMD). Symptoms can include:
- Jaw pain or soreness, especially in the morning or after chewing
- Clicking, popping, or grating sounds when you open your mouth
- Locking of the jaw joint
- Headaches that feel like tension headaches, often around the temples
- Earaches or a feeling of fullness in the ears
Chewing efficiency takes a hit too. It's harder to bite into an apple or a sandwich cleanly. You might find yourself favoring one side of your mouth, which leads to uneven muscle development and more strain.
Speech can be affected. Certain sounds, like "f," "v," "s," and "th," require precise contact between the teeth, tongue, and lips. An underbite can make these sounds lispy or less clear.
And yes, the psychological side is real. It's not vanity.
Feeling self-conscious about your profile or smile can affect social interactions, confidence, and even career opportunities. It's a quality-of-life thing that shouldn't be dismissed. The American Association of Orthodontists has resources that discuss the psychosocial benefits of correcting dental issues, which go beyond a straight smile.
Your Treatment Roadmap: From Braces to Surgery
Figuring out how to fix an underbite depends on one crucial factor: is it a dental problem or a skeletal problem?
A dental underbite means the teeth are tilted or positioned in a way that creates the underbite, but the jawbones themselves are in a fairly normal relationship. A skeletal underbite means the jawbones – the actual foundation – are mismatched in size or position. Most adult underbites have a skeletal component. This distinction dictates everything.
For Kids and Teens (When Growth is on Your Side)
Treatment in younger patients aims to guide growth. It's about steering the train, not rebuilding the tracks later. The goal is to encourage the upper jaw to grow forward and/or restrain the forward growth of the lower jaw.
- Upper Jaw Expanders (Palatal Expanders): A common first step. This device is fixed to the upper molars and has a screw in the middle. Turned with a key, it gently widens the upper jaw over weeks or months. This can create space for crowded teeth and, in some cases, improve the bite relationship. It sounds medieval, but it's highly effective for certain types of underbites.
- Reverse-Pull Face Mask (Face Mask Therapy): This looks more intimidating than it is. It's a headgear with pads that rest on the forehead and chin, connected by a framework that pulls the upper jaw forward. Worn at night and for several hours during the day, it uses the child's own growth to reposition the upper jaw. The key is timing – it works best before a growth spurt, usually between ages 8 and 11.
- Functional Appliances: Devices like the Twin Block or a Frankel III appliance sit in the mouth and reposition the lower jaw backward, encouraging the upper jaw to grow while holding the lower jaw in a new position. They rely on muscle function and growth to make changes.
For Adults (When the Growth Trains Have Left the Station)
Once growth is complete (late teens for girls, late teens/early 20s for guys), you can't guide jaw growth anymore. Now you're looking at camouflage or surgery.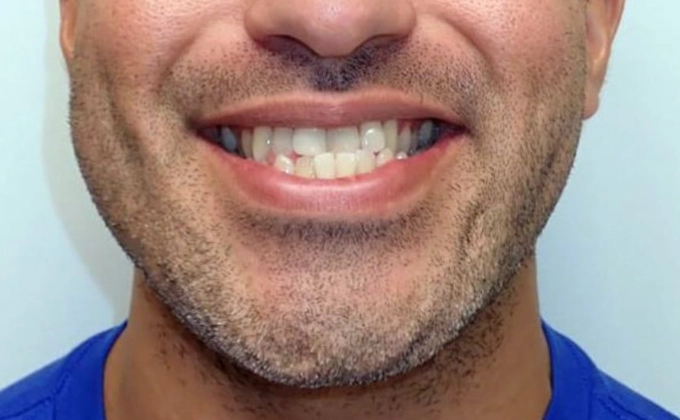
Camouflage Orthodontics: This is for mild to moderate skeletal underbites. The goal isn't to fix the jaw position, but to move the teeth in such a way that they meet properly despite the jaw mismatch. It usually involves braces or clear aligners to tip the upper teeth forward and the lower teeth backward. It can create a great functional bite and a much-improved appearance, but it doesn't change the underlying jaw structure. Your profile might improve, but not as dramatically as with surgery. There's also a limit – if the skeletal discrepancy is too large, trying to camouflage it can make the teeth stick out too far and look unstable.
Orthognathic Surgery (Jaw Surgery): This is the definitive treatment for a moderate to severe skeletal underbite. It's a collaboration between an orthodontist and an oral & maxillofacial surgeon. The process has distinct phases:
- Pre-surgical Orthodontics (12-18 months): Braces are put on to first decompensate the teeth. This means moving them into their natural, but now worse, positions relative to their own jaws. Your underbite will actually look more pronounced right before surgery. This is necessary so the jaws can be moved into their correct positions with the teeth fitting together perfectly at the end.
- The Surgery: The surgeon makes precise cuts in the jawbones (osteotomies) and repositions them. For an underbite, the most common procedure is a maxillary advancement (moving the upper jaw forward), often combined with a mandibular setback (moving the lower jaw backward). Plates and screws hold everything in the new position while it heals. You can find detailed, peer-reviewed information on these surgical procedures from sources like the American Association of Oral and Maxillofacial Surgeons (AAOMS).
- Recovery: The first week or two involves swelling, a liquid/soft diet, and rest. Most people feel significantly better after 2-3 weeks and return to normal activities within 6-8 weeks, though full healing of the bone takes months.
- Post-surgical Orthodontics (6-9 months): Fine-tuning the bite with braces after everything has settled.
Surgery is a big deal. But for the right person, the results are life-changing.
| Treatment Option | Best For | How It Works | Pros | Cons / Things to Know |
|---|---|---|---|---|
| Camouflage Orthodontics (Braces/Aligners) | Mild skeletal or dental underbites in adults/teens | Tips teeth to meet correctly without moving jaws. | Non-surgical. Shorter overall timeline. Less invasive. | Doesn't change jaw profile. Limited by severity. May compromise tooth position long-term if overdone. |
| Jaw Surgery (Orthognathic) | Moderate to severe skeletal underbites in adults | Physically repositions the upper and/or lower jawbones. | Corrects the root cause. Improves facial profile and function dramatically. Permanent skeletal solution. | Major surgery with recovery time. Requires pre- and post-surgical braces. Higher cost and complexity. |
| Early Intervention (Expanders, Face Masks) | Growing children (ages 7-11) with developing underbites | Guides jaw growth using the child's own growth potential. | Can prevent need for surgery later. Less invasive than adult options. | Requires good compliance from child. Timing is critical. Doesn't work for all cases. |
How to Choose Your Path and Find the Right Help
This is where many people get stuck. Do you see an orthodontist? A surgeon? Your regular dentist? The process starts with a solid diagnosis.
Step 1: The Comprehensive Evaluation. Any good specialist will start here. This isn't just a quick look in your mouth. It should include:
- Photographs of your face and teeth.
- Digital or plaster models of your teeth.
- A panoramic X-ray to see all teeth and jaws.
- A cephalometric X-ray. This is the key one. It's a side-view X-ray of your skull that allows precise measurements of jaw positions, tooth angles, and facial proportions. This analysis tells the expert if your underbite is skeletal, dental, or both, and by how many millimeters.
- Sometimes, a 3D cone-beam CT scan for complex surgical cases.
Step 2: The Consultations. For a suspected skeletal underbite, you need a board-certified orthodontist involved. Full stop. They are the quarterbacks of bite correction. They will diagnose the type and severity and map out the orthodontic plan.
If surgery is on the table, the orthodontist will refer you to a board-certified oral and maxillofacial surgeon for a joint consultation. Don't skip this. The surgeon will examine you, review the records, and discuss the surgical procedure, risks, benefits, and recovery in detail. You should leave this consultation with a clear mental movie of the entire process.
Correcting an underbite, whether with braces or surgery, is a journey. It requires patience, trust in your clinical team, and a clear understanding of your own goals. Are you seeking perfect function? Aesthetic change? Relief from pain? Be clear about that with your doctor. The technology and expertise are there to help. The first step is simply understanding what you're dealing with, and I hope this guide has helped shine a light on the path forward.