Quick Guide
Let's be honest, finding a strange spot in your mouth is unsettling. You're brushing your teeth, and there it is—a patch on your gum that wasn't there before. Your mind races. Is it just an irritation? A canker sore? Or could it be something more serious? The question "What do cancerous gum lesions look like?" isn't just a medical query; it's often a quiet, anxious thought in the back of someone's mind. I get it. The internet is full of scary images and vague descriptions that either downplay the risk or send you into a panic. My aim here is to cut through that noise. We'll walk through exactly what to look for, using clear descriptions (no overly graphic photos, promise), and, more importantly, we'll talk about what to do next. Knowledge is your first and best line of defense.
First, a crucial point I need to stress: I'm not a doctor. This guide is based on information from reputable health organizations and is meant to educate and empower you. It is not a substitute for a professional examination. If you see anything in your mouth that matches the descriptions below and doesn't go away within two weeks, please, book an appointment with your dentist or doctor. Don't wait. Don't Google yourself into a frenzy. Just get it checked.
Breaking Down the Appearance: A Visual Checklist
So, what do cancerous gum lesions look like in reality? They don't have one uniform appearance, which is partly why they can be tricky. However, they often present with a combination of features. Think of this as a checklist, not a diagnosis. The presence of several of these traits increases the need for a check-up.
Color Changes: The Red, White, and Mixed Flags
Your healthy gum tissue (gingiva) is generally a uniform coral pink, though color can vary with skin tone. Cancerous changes often disrupt this uniformity.
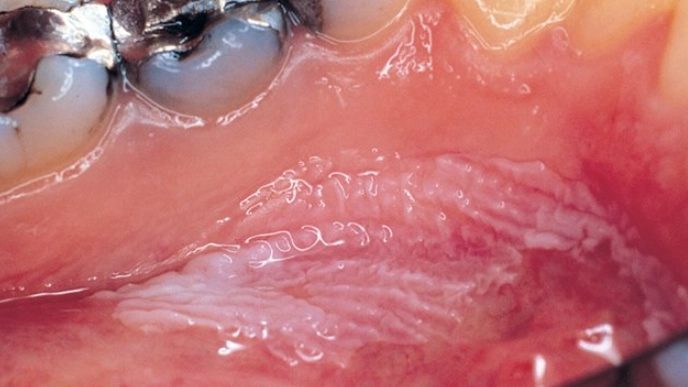
- Leukoplakia (White Patches): This is a classic warning sign. It appears as a firmly attached, white or greyish patch that cannot be scraped off. It often feels rough or leathery. Now, crucial detail—most leukoplakia is benign. But a subset can be precancerous or already harbor cancerous cells. The risk is higher if the patch has red areas mixed in (called "speckled leukoplakia"). When wondering what do cancerous gum lesions look like, these persistent, non-wipeable white patches are a top contender for needing a biopsy.
- Erythroplakia (Red Patches): This is less common but far more concerning. It appears as a bright red, velvety patch that is often flat or slightly depressed. Unlike an inflamed area from gum disease, erythroplakia is typically well-defined and persists. Dentists and oral surgeons view erythroplakia with high suspicion because a significant percentage of these lesions are either severely precancerous or cancerous at discovery.
- Erythroleukoplakia (Mixed Red & White Patches): As the name suggests, this is a mix. It looks like a white patch with intermixed or speckled red areas. This mixed appearance is considered a higher-risk indicator than a uniform white patch alone.
Shape, Texture, and Sensation
It's not just about color. How the lesion feels and its structure are huge clues.
- Ulcers and Sores: A classic cancer sign is an ulcer that doesn't heal. It might have raised, rolled borders and a crater-like center. The base may be necrotic (dead tissue), looking yellowish or greyish.
- Lumps and Thickening: You might feel a lump or a general area of thickening on your gum with your tongue. The tissue may feel hard or indurated. This growth can sometimes be wart-like or cauliflower-shaped.
- Texture Changes: The surface might become rough, crusty, or develop a verrucous (warty) appearance. Normal mucosa is smooth and uniform.
- Bleeding: The lesion might bleed spontaneously, without any provocation like brushing or eating. This isn't the generalized bleeding of gingivitis but localized bleeding from the specific spot.
- Loosening of Teeth or Numbness: As a lesion grows, it can affect underlying structures. You might notice a tooth becoming loose for no apparent dental reason (like gum disease or trauma). There could also be numbness or a tingling sensation in the area.
Here’s a quick comparison table to help differentiate common gum issues. Remember, this is for guidance only.
| Feature | Common Canker Sore (Aphthous Ulcer) | Gingivitis/Periodontitis | Potential Cancerous Gum Lesion |
|---|---|---|---|
| Pain | Often quite painful. | Gums may be tender, bleed easily. | May be painless in early stages. Pain can develop later. |
| Duration | Heals within 7-14 days. | Chronic condition, but inflammation can come and go. | Persists for more than 2 weeks without healing. |
| Appearance | Round/oval with a white/yellow center and red halo. Shallow. | Generalized red, swollen, shiny gums. Receding gums in periodontitis. | Variable: white/red/mixed patch, non-healing ulcer with rolled edges, lump. |
| Borders | Well-defined but not raised or hardened. | Diffuse, affects a wide area along the gumline. | May be irregular, raised, rolled, or hard. |
| Bleeding | May bleed if irritated. | Bleeds easily, especially when brushing/flossing. | May bleed spontaneously without cause. |
See the difference? Persistence and change are key. A canker sore is a nuisance but follows a predictable healing path. Gum disease is widespread. A potential cancerous lesion is a localized, persistent change that breaks the normal rules.
Where Do They Typically Show Up?
Location matters. While oral cancer can occur anywhere, certain sites are more common. On the gums (gingiva), lesions are frequently found on the lower gum behind the lower back teeth (the retromolar trigone area) and along the gumline. However, they can appear on the upper gums, the roof of the mouth (palate), or the inner cheek lining adjacent to the gums. The takeaway? Check everywhere during your self-exam, but pay extra attention to areas that are harder to see.
What Happens at the Dentist? The Diagnosis Process
Let's say you've seen something concerning. What's next? Understanding the process can reduce anxiety.
- Clinical Examination: Your dentist will do a thorough visual and tactile exam of your entire mouth, neck, and throat. They'll feel for lumps in your neck (lymph nodes). They'll use a bright light and possibly a special rinse or light to highlight abnormal tissue. The VELscope, for example, uses fluorescent light to show changes not visible to the naked eye, though it's an aid, not a definitive test.
- Medical History Review: They'll ask about your habits (tobacco, alcohol), sun exposure (for lip lesions), and overall health. This context is vital.
- The Biopsy: This is the only way to definitively answer the question "Is this cancerous?" If a lesion is suspicious, the dentist or an oral surgeon will recommend a biopsy. A small sample of tissue is taken (usually with local anesthesia) and sent to a pathology lab. The pathologist examines the cells under a microscope. Types include incisional (taking a piece) or excisional (removing the whole lesion). It sounds scarier than it is—it's a routine procedure.
Waiting for biopsy results is the hardest part. But knowing the process helps. The goal is to get a clear answer so you can have a clear path forward.
Common Questions People Are Afraid to Ask
Let's tackle some of the quiet, nagging questions that come up when you're searching for "what do cancerous gum lesions look like."
- Pull your lips and cheeks out to see the front and back of your gums.
- Tilt your head back to check the roof of your mouth and upper gums.
- Stick out your tongue and check its sides and underneath.
- Feel all around with a clean finger for lumps, bumps, or rough areas.
- Look for the color, texture, and shape changes we discussed.
- Tobacco Use: This is the #1 risk factor—smoking, chewing, snuff. All forms.
- Heavy Alcohol Use: Especially combined with tobacco, which multiplies the risk.
- Human Papillomavirus (HPV): HPV-positive oropharyngeal cancer is rising, but it typically affects the tonsils and base of the tongue, less commonly the gums directly. Still, it's a major overall oral cancer cause.
- Sun Exposure: For cancers on the lips, which can extend to the gums.
- Age & Gender: Risk increases with age, and men are affected more than women.
Quick-Action Summary: When to See a Professional
- Any white, red, or mixed patch that does not wipe off and persists for >2 weeks.
- Any ulcer or sore that does not heal within 2 weeks.
- Any lump, thickening, or rough spot on the gum.
- Unexplained bleeding from a specific spot in the mouth.
- Unexplained numbness or loosening of teeth.
- A persistent feeling that something is caught in your throat.
- Even if you have just one of these signs and are unsure, get it checked. It's what your dentist is there for.
If It Is Cancer: Understanding the Path Forward
This is the part no one wants to think about, but information dispels fear. If a biopsy confirms cancer (often called oral squamous cell carcinoma when it starts in the lining tissues), treatment has come a long way.
Treatment is highly individualized but often involves:
- Surgery: To remove the tumor with a margin of healthy tissue. For gum cancers, this might involve removing a portion of the jawbone (mandibulectomy or maxillectomy), which can be reconstructed.
- Radiation Therapy: Used alone for early stages or after surgery to kill any remaining cancer cells.
- Chemotherapy: Often used in combination with radiation (chemoradiation) for more advanced cases.
- Targeted Therapy & Immunotherapy: Newer drugs that target specific aspects of cancer cells or boost your immune system to fight the cancer.
The prognosis depends heavily on the stage at diagnosis. This is why answering "what do cancerous gum lesions look like" early is so powerful. Early-stage (I & II) oral cancers have significantly higher survival and cure rates, often with less aggressive treatment. Late-stage (III & IV) is much harder to treat. That two-week rule isn't arbitrary; it's about catching things at stage I, not stage IV.
For comprehensive, trustworthy information on treatment options and support, the National Cancer Institute's section on head and neck cancers is an authoritative source.
Final Thoughts: Empowerment Over Fear
Look, the goal of this article isn't to scare you. It's the opposite. Fear comes from the unknown. Now, you know what to look for. You know that a persistent change is your cue to act, not to hide. You know the process. You know that early detection changes everything.
So, what do cancerous gum lesions look like? They look like change. They look like persistence. They look like something that doesn't belong.
Your mouth is a resilient place, but it's not invincible. Pay attention to it. See your dentist for regular check-ups—they are trained to spot these things often before you even notice them. And if you see something, don't let embarrassment or fear of "wasting the doctor's time" stop you. Getting a clean bill of health is a win. Catching something early is a life-saving win.
Take that knowledge and use it. Be proactive about your health. It's the most important thing you own.