Let's be honest. When most people hear "orthodontic surgery," they picture a purely cosmetic procedure for a perfect Hollywood smile. I've been in the field for over a decade, and that's the biggest misconception I correct daily. The truth is, surgical orthodontics, or orthognathic surgery, is often less about vanity and more about fundamental quality of life. It's for people whose bite problems are so severe that braces alone can't fix them. We're talking about difficulties that affect breathing, chewing, speaking, and even sleeping.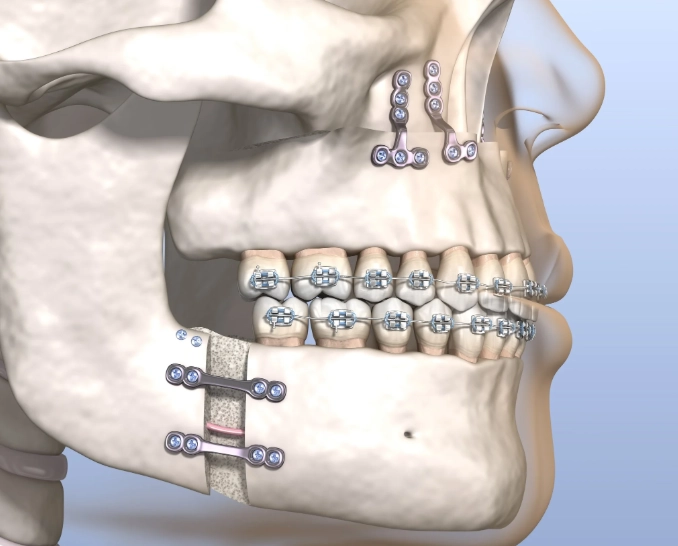
I've seen patients who lived with chronic jaw pain for years, thinking it was just normal tension. Others struggled with sleep apnea because their airway was physically restricted by their jaw structure. This guide isn't about selling you on surgery. It's about giving you the unfiltered, detailed information you need to understand if it's the right path for you, what it truly involves, and how to navigate the journey successfully.
What You’ll Find in This Guide
What Exactly Is Orthognathic Surgery?
Orthognathic surgery is a procedure performed by an oral and maxillofacial surgeon to reposition the jaws. It's almost always done in combination with orthodontic treatment (braces or aligners). Think of it this way: the orthodontist moves the teeth into their correct positions within each jaw, and the surgeon moves the entire jaw bones themselves so that those teeth can meet properly.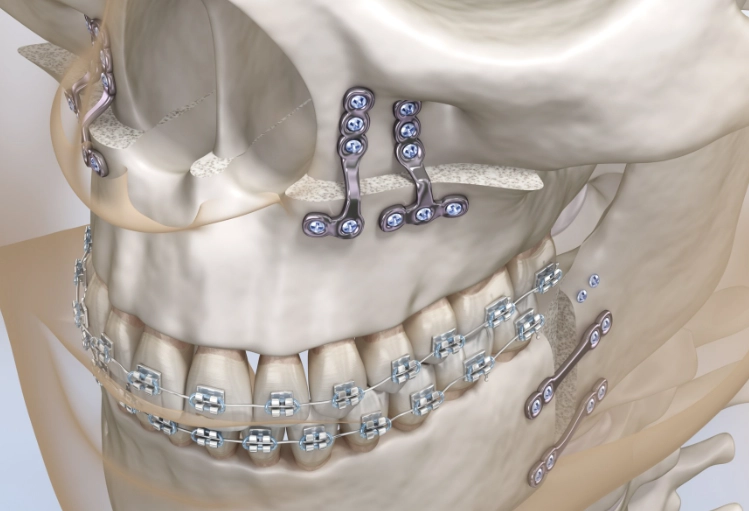
The goal is to create a functional bite, improve facial balance, and resolve issues caused by significant jaw misalignment. It's major surgery, requiring general anesthesia and a hospital stay, but the functional improvements can be life-changing.
Who Actually Needs Jaw Surgery?
This isn't for minor overbites. Candidates typically have skeletal discrepancies that can't be camouflaged with orthodontics alone. Common indicators include:
- Severe Underbite (Class III Malocclusion): The lower jaw protrudes far forward of the upper jaw.
- Severe Overbite/Overjet (Class II Malocclusion): The upper jaw is too far forward, or the lower jaw is too far back, sometimes making the chin appear weak.
- Open Bite: The front teeth don't touch when the back teeth are together, often making it impossible to bite through foods like a sandwich.
- Asymmetry: One side of the jaw grows more than the other, leading to a facial imbalance.
- Obstructive Sleep Apnea: Caused by a small or recessed lower jaw that blocks the airway during sleep.
- Chronic Jaw (TMJ) Pain: Or difficulty chewing that stems from the jaw joint being under excessive strain due to the misalignment.
If you're constantly biting the inside of your cheeks, have speech issues, or experience unexplained headaches, a jaw discrepancy could be the root cause. A consult with an orthodontist and surgeon is the only way to know for sure.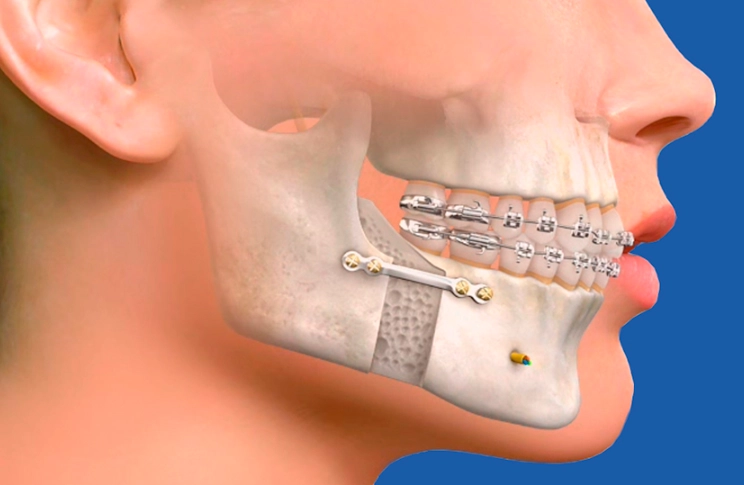
The Different Types of Jaw Surgery Procedures
The specific surgery depends on your unique anatomy. Here’s a breakdown of the most common procedures.
Upper Jaw Surgery (Maxillary Osteotomy)
This involves moving the entire upper jaw. It can be moved forward, backward, up, or down. It's often used to correct open bites, severe overbites, or to level a smile line that's uneven due to a canted jaw.
Lower Jaw Surgery (Mandibular Osteotomy)
The most common version is the Bilateral Sagittal Split Osteotomy (BSSO). Sounds intense, but it's the standard for moving the lower jaw forward or backward. The surgeon makes cuts on both sides of the jawbone behind the molars, allowing the front segment (holding your teeth) to be repositioned while maintaining connection to the jaw joint.
Double Jaw Surgery (Bimaxillary Osteotomy)
This is when both the upper and lower jaws are repositioned. It's for the most complex cases to achieve optimal facial balance and function. The planning for this is incredibly precise, using 3D surgical simulations.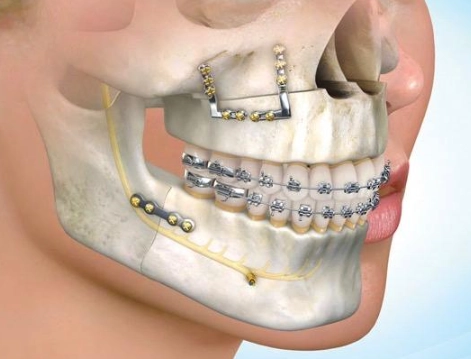
Genioplasty (Chin Surgery)
Sometimes performed alone or in conjunction with other procedures. It adjusts the position of the chin bone to improve profile aesthetics. It's important to note that genioplasty alone doesn't fix a bad bite.
A Note from Experience: One subtle error I see in online forums is the conflation of genioplasty with orthognathic surgery. Adding a chin implant might improve the look of a recessed jaw, but it does nothing to address the underlying skeletal problem, the airway issue, or the dysfunctional bite. It's a cosmetic add-on, not a functional solution. Always address the root skeletal cause first.
The Complete Process: From Consultation to Recovery
This isn't a quick fix. The full journey typically spans 2-3 years. Understanding each phase manages expectations.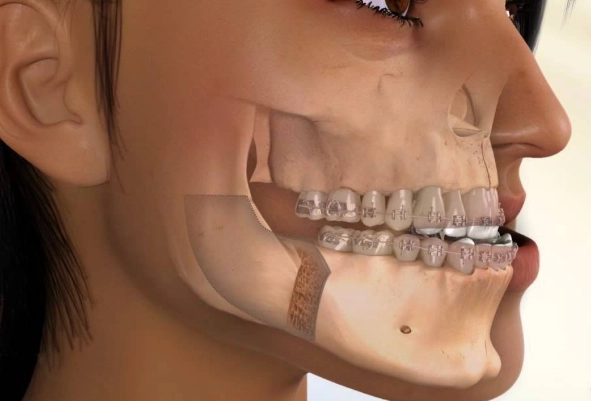
Phase 1: Pre-Surgical Orthodontics (12-18 months)
You'll get braces or start Invisalign treatment. This seems backward—why make your bite worse before surgery? The orthodontist is decompensating your bite. They're moving your teeth into their ideal positions within each misaligned jaw. So, an underbite might become more pronounced. This is normal and crucial for the surgeon to have optimal bone to work with.
Phase 2: Surgical Planning & The Procedure
Planning involves photos, X-rays, and a 3D CT scan. Your surgical team will use software to simulate the exact bone movements. The surgery itself takes several hours. You'll be under general anesthesia in a hospital. The surgeon makes incisions inside the mouth (so no visible scars), makes precise cuts in the jawbones, repositions them using custom surgical guides, and secures them with tiny plates and screws.
Phase 3: Post-Surgical Orthodontics (6-12 months)
After healing (about 4-6 weeks), orthodontic treatment resumes to fine-tune your bite and settle the teeth into their new, perfect positions. This final detailing phase is what gives you that great functional and aesthetic result.
A Realistic Recovery Timeline (Week by Week)
Recovery is the part everyone worries about most. Let's get real about what it's like.
| Time Period | What to Expect | Key Focus & Tips |
|---|---|---|
| Week 1-2 | Significant swelling, bruising, numbness. Liquid diet only (broths, protein shakes). Discomfort managed with medication. You'll be tired. | Rest, ice packs (20 mins on/20 off), hydration. Use a syringe or squeeze bottle to eat. Keep head elevated. |
| Weeks 3-4 | Major swelling subsides. Transition to "no-chew" soft foods (mashed potatoes, yogurt, scrambled eggs). Numbness may persist. Energy starts to return. | Begin very gentle jaw exercises as directed. Focus on nutrition. Start rinsing gently with warm salt water. |
| Weeks 5-8 | Swelling continues to decrease slowly. Can progress to soft foods that require minimal chewing (pasta, soft fish). Most people return to work/school. | Gradually increase jaw mobility exercises. Final appearance begins to emerge. Follow-up with surgeon. |
| Months 3-6 | 90% of swelling is gone. Can usually eat most foods, but avoid very hard or chewy items. Numbness in lips/chins may slowly improve over years. | Resume normal activities. Orthodontics reactivates. Sensation returns gradually. |
The mental and emotional aspect of recovery is huge. You'll look different in the mirror, and your face feels strange and swollen. Having a support system and preparing mentally for this temporary phase is as important as the physical prep.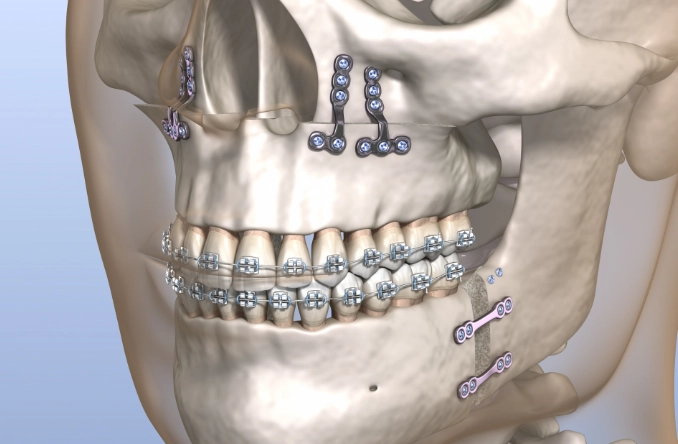
Costs, Insurance, and Hidden Expenses
Costs vary wildly by region, surgeon, and case complexity. In the US, total costs (surgeon, hospital, anesthesia, orthodontics) can range from $20,000 to $70,000+.
The big question: Will insurance cover it? Often, yes, if it's deemed medically necessary. Insurance companies have specific criteria (like a certain millimeter discrepancy measured on X-rays, documented sleep apnea, or functional impairment). Your surgeon's office will handle the pre-authorization process, submitting clinical notes, photos, and X-rays to prove medical necessity.
Hidden costs people forget:
- Pre-surgical dental work: You may need cavities filled or a deep cleaning before braces.
- Time off work: Budget for at least 2-4 weeks of unpaid leave if you don't have sufficient sick/vacation time.
- Post-surgery nutrition: Protein shakes, supplements, and soft foods can add up.
- Medications: Prescription pain meds and antibiotics.
- Follow-up appointments: Travel and potential time off for numerous check-ups.
Leave a Reply