Key Takeaways for Quick Reading
- Spotting the Signs: Is It Really a Dental Abscess?
- What to Do Right Now: Emergency Steps Before You See the Dentist
- The Professional Fix: What Actually Happens at the Dentist
- Comparing Your Treatment Paths
- Life After the Abscess: Healing and Making Sure It Doesn't Come Back
- Your Dental Abscess Questions, Answered
Let's talk about one of the most urgent and frankly, miserable, problems you can have in your mouth: a dental abscess. If you've never had one, count yourself lucky. If you're reading this because you suspect you might have one right now, I feel for you. That deep, throbbing pain is unlike any regular toothache. It's your body sending a serious flare-up signal that something is very wrong beneath the surface.
I remember a friend describing his experience before he finally went to the dentist. He said it felt like a tiny, angry construction worker was inside his jawbone, hammering away with a predictable, brutal rhythm. He tried every home remedy in the book, which, spoiler alert, did almost nothing. That's the thing about a dental abscess – it's an infection that's walled itself off, and it's not going away without professional intervention.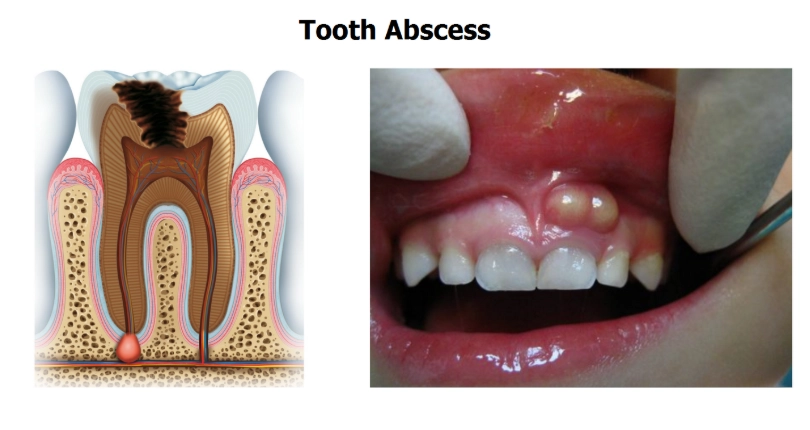
So, what exactly are we dealing with? In simple terms, a dental abscess is a localized collection of pus caused by a bacterial infection. Think of it as a boil, but inside your tooth or gums. This pus-filled pocket creates pressure, and since it's in a confined space (your jaw), that pressure translates directly into pain. The bacteria usually get in through a cavity, a crack in the tooth, or advanced gum disease.
Here's the critical part a lot of people miss: a dental abscess is an infection that can spread. It doesn't just stay in your tooth. If left untreated, the bacteria can move into your jawbone, your soft facial tissues, and in rare but severe cases, into your bloodstream or other areas of your head and neck. This can become life-threatening. So, treating a tooth abscess isn't just about pain relief; it's about preventing a local problem from becoming a systemic health crisis.
Spotting the Signs: Is It Really a Dental Abscess?
How do you know it's an abscess and not just a bad cavity or sensitive tooth? The symptoms tend to be a package deal, and they're pretty distinctive once they all show up.
The headline symptom is pain. But not just any pain. It's often described as:
- A persistent, throbbing ache that can radiate to your jawbone, neck, or ear.
- Pain that gets worse when you lie down, due to increased blood pressure to the head.
- Sharp or shooting pain when you apply pressure to the tooth, like when chewing.
Then come the other guests to this unpleasant party. You might notice sudden sensitivity to hot and cold temperatures that lingers long after the source is gone. Your gums around the tooth may become red, swollen, and shiny. In some cases, the swelling can be significant, causing your face to look puffy on one side. You might even be able to see or feel a pimple-like bump on your gums near the root of the tooth – that's a draining fistula, and it's a classic sign of a tooth abscess trying to release pressure.
Don't ignore these: A foul, salty, or metallic taste in your mouth (that's the pus draining), swollen or tender lymph nodes under your jaw or in your neck, and even a general feeling of being unwell or running a fever. Fever is a red flag that the infection may be spreading beyond the localized abscess.
It's also helpful to know there are different types, which start in different places. A periapical abscess happens at the very tip of the tooth's root, usually from an untreated cavity or trauma that lets bacteria infect the pulp (the tooth's nerve center). A periodontal abscess starts in the supporting bone and gum tissues next to the tooth root, often from advanced gum disease. The treatment approach can differ slightly based on the type.
What to Do Right Now: Emergency Steps Before You See the Dentist
Okay, you've identified the likely culprit. Your mouth is screaming, and your dentist's office is closed. What can you actually do that helps?
First, let's talk about pain management. Over-the-counter pain relievers like ibuprofen (Advil) or naproxen (Aleve) can help reduce both pain and inflammation. Acetaminophen (Tylenol) can help with pain but doesn't tackle inflammation. Always follow the dosage instructions on the label. A cold compress or ice pack wrapped in a cloth and held against the outside of your cheek for 15-minute intervals can also numb the area and reduce swelling.
Now, about rinsing. A warm saltwater rinse (half a teaspoon of salt in a cup of warm water) can be surprisingly soothing. It helps clean the area, draw out some fluid, and temporarily reduce bacteria. Do this gently several times a day. Some people swear by rinsing with a diluted hydrogen peroxide solution, but you have to be careful not to swallow it, and it can irritate gums. Personally, I think salt water is simpler and safer for most people in a pinch.
I need to be blunt about something I see online all the time: “natural” remedies like garlic, clove oil, or tea bags placed on the gum. Do they sometimes provide temporary, mild numbing? Sure. Do they cure the abscess? Absolutely not. At best, they're a distraction. At worst, they can irritate the tissue further or give you a false sense of security while the infection worsens. Never put aspirin directly on the gum or tooth—it can burn your tissue.
Adjust your habits. Try to sleep with your head elevated on an extra pillow. This helps reduce the throbbing pressure. Stick to soft, cool foods (yogurt, applesauce, smoothies) and avoid chewing on that side of your mouth completely. And please, avoid extreme temperatures—no scorching hot coffee or ice-cold water directly on the tooth.
The Professional Fix: What Actually Happens at the Dentist
This is the only part that actually solves the problem. Home care is just damage control until you get professional help. When you see your dentist or an endodontist (root canal specialist), their primary goals are to drain the infection, remove the source of the bacteria, and save the tooth if possible.
The first step is diagnosis. They'll examine your tooth, tap on it, and likely take an X-ray. The X-ray is crucial—it shows the extent of the infection in the bone and helps confirm the type of dental abscess. Once confirmed, here are the main routes they might take:
Incision and Drainage (I&D)
This is often the first in-office procedure to get immediate relief. The dentist makes a small cut in the gum to let the pus drain out. The pressure release is almost instant, and the pain drops dramatically. They'll then flush the area with a saline solution. Sometimes a small rubber drain is left in place for a day or two to ensure all the infection drains out.
Root Canal Treatment
This is the gold standard for saving a tooth with a periapical abscess. The idea freaks a lot of people out, but modern root canals are typically no more uncomfortable than getting a filling. The dentist removes the infected or dead pulp from inside the tooth, meticulously cleans and disinfects the inner chambers (the root canals), and then fills and seals them. Finally, a crown is usually placed on the tooth to restore its strength. This procedure removes the bacteria's home and seals the tooth off from future infection. The American Association of Endodontists has a great patient resource on this process that demystifies it.
Tooth Extraction
Sometimes, the tooth is too damaged or broken to be saved. If saving it isn't feasible, the dentist will recommend an extraction. They remove the tooth and thoroughly clean the socket. While losing a tooth isn't ideal, removing the source of the infection is paramount. You can discuss replacement options like bridges or implants later, once the infection has fully cleared.
Antibiotics are a supporting actor in this drama, not the star. They don't cure the abscess on their own because they can't effectively penetrate the wall of the abscess to kill all the bacteria inside. However, dentists prescribe them in specific situations: if the infection has spread to surrounding tissues, if you have a weakened immune system, or if you have systemic symptoms like a fever. The CDC provides guidelines on the appropriate use of antibiotics in dentistry, which responsible dentists follow to combat antibiotic resistance.
Comparing Your Treatment Paths
It can be confusing to understand which treatment is for which scenario. This table breaks down the common options, their goals, and what to expect.
| Treatment | Best For | What It Does | Long-Term Outcome |
|---|---|---|---|
| Incision & Drainage (I&D) | Immediate relief from a large, painful abscess. Often a first step. | Releases pus and pressure directly from the gum abscess. | Provides immediate pain relief but does not fix the underlying cause. Further treatment (root canal or extraction) is always needed. |
| Root Canal Therapy | A salvageable tooth with an infected pulp (periapical abscess). | Removes infected inner tissue, cleans, seals the tooth, and is topped with a crown. | Saves the natural tooth. With proper care, it can last a lifetime. |
| Tooth Extraction | A severely damaged, non-restorable tooth, or patient preference. | Removes the entire source of the infection (the tooth). | Eliminates infection but creates a gap. Requires discussion of replacement options (implant, bridge, partial denture). |
| Periodontal Treatment | A periodontal abscess from gum disease. | Deep cleaning (scaling/root planing) below the gumline to remove tartar and bacteria. | Manages gum disease and the abscess. Requires ongoing periodontal maintenance. |
Life After the Abscess: Healing and Making Sure It Doesn't Come Back
You've had the treatment. The pain is gone. Now what? The healing process is crucial, and your long-term habits are what will prevent another dental abscess from forming somewhere else.
Right after a procedure like a drainage or root canal, follow your dentist's post-op instructions to the letter. This usually means:
- Taking any prescribed medications (like antibiotics) as directed, even if you feel better.
- Using over-the-counter pain meds as needed for any residual soreness.
- Sticking to soft foods for a day or two.
- Practicing gentle oral hygiene around the area.
- Watching for signs of complications (increased swelling, fever, severe pain) and calling your dentist immediately if they occur.
But the real work is long-term prevention. A tooth abscess is almost always the result of a problem that was ignored. So, your new dental defense plan should be airtight.
The Prevention Checklist:
- Brushing & Flossing: Non-negotiable. Brush twice daily with fluoride toothpaste and floss once a day to remove plaque between teeth.
- Regular Dental Visits: See your dentist for check-ups and cleanings at least twice a year. They catch small cavities and gum issues long before they turn into an abscess.
- Fix Problems Early: That tiny cavity? Get it filled now. Don't wait for it to become a big, painful problem.
- Protect Your Teeth: If you play sports, wear a mouthguard. If you grind your teeth at night (bruxism), talk to your dentist about a night guard. Cracks from trauma or grinding are a direct pathway for bacteria.
- Mind Your Diet: Limit sugary and acidic foods and drinks. They fuel the bacteria that cause decay and gum disease. The Mayo Clinic outlines the clear link between diet and tooth decay.
- Don't Smoke: Smoking severely compromises your gum health and immune response, making infections more likely and harder to heal.
Think of it this way: an abscess is a loud, painful alarm bell. You can either hit snooze with temporary measures and face a bigger disaster later, or you can answer the call and use it as a wake-up call to finally take your oral health seriously.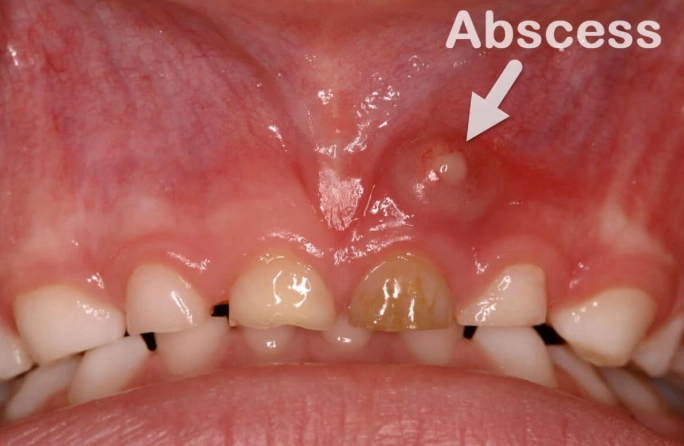
Your Dental Abscess Questions, Answered
Can a dental abscess go away on its own?
No. The infection might occasionally drain through the gum, which can temporarily relieve pain and pressure. This can fool you into thinking it's healing. But the source of the infection—the bacteria inside the tooth or deep in the gum pocket—is still there. It will almost certainly flare up again, often worse than before. Professional treatment is the only way to resolve it permanently.
How urgent is a tooth abscess? Is it a dental emergency?
Yes, it should be treated as a dental emergency. You should call your dentist as soon as you suspect one. While you may not need to go to the hospital ER immediately if symptoms are mild, delaying treatment for days or weeks allows the infection to spread and can make treatment more complex. Severe swelling in your face or floor of your mouth, difficulty breathing or swallowing, or a high fever are signs to seek emergency medical care immediately.
What happens if an abscess bursts in your mouth?
You'll likely get a sudden rush of foul-tasting, salty fluid (pus). The pressure and pain may decrease significantly, which feels like relief. However, this is not a cure. You must still see a dentist. The fistula (draining hole) may close, trapping bacteria inside again, leading to another buildup. The underlying infection is still active and needs to be treated.
How long can you have a dental abscess before it becomes dangerous?
There's no safe timeline. The risk isn't just about time, but about the virulence of the bacteria and your body's immune response. An abscess can start causing damage to the surrounding bone within days. The potential for it to spread to other areas, while rare, is a constant risk once the infection is established. The sooner you get it treated, the lower all these risks become.
Is a dental abscess contagious?
The condition itself isn't contagious like a cold. You can't “catch” an abscess from someone. However, the bacteria that cause dental infections can be spread through saliva (e.g., sharing utensils, drinks, or kissing). If someone else has poor oral health or an open sore in their mouth, those bacteria could potentially contribute to their own dental problems. It's always good practice to maintain general hygiene.
Look, dental problems are stressful. They're painful, expensive, and disruptive. But ignoring a dental abscess is one of the worst things you can do. It turns a manageable problem into a major one.
The takeaway is simple: if you have the signs, get it checked out. Don't rely on Dr. Google and a bottle of clove oil. Modern dentistry has incredibly effective ways to treat a tooth abscess, eliminate your pain, and save your smile. Use this experience as a catalyst. Book that cleaning you've been putting off, floss tonight, and make peace with your dentist. Your future self will thank you.