Quick Navigation Guide
- How Do You Even Know You Have It? Diagnosis Comes First.
- The Core of Porphyromonas Gingivalis Treatment: Professional Intervention
- The Antibiotics Question: To Use or Not to Use?
- Your Role At Home: The Treatment Doesn't End at the Dentist's Door
- What Does Success Look Like? Monitoring and Maintenance
- Common Questions People Are Afraid to Ask
- Putting It All Together: A Realistic Action Plan
Let’s talk about Porphyromonas gingivalis. If you’re reading this, you’ve probably heard the name, maybe from your dentist, and you’re now staring down a search for Porphyromonas gingivalis treatment options. It sounds intimidating, like some kind of medieval plague. Honestly, it kind of is for your gums. This isn’t just any mouth bacteria; it’s a prime suspect, the ringleader, in the messy, destructive process of periodontitis—the severe gum disease that can lead to tooth loss. The good news? It can be managed. The better news? You’re about to get a no-nonsense, detailed breakdown of exactly how.
So, what are we dealing with? P. gingivalis isn’t just a passive resident. It’s a keystone pathogen. That’s a fancy way of saying it doesn’t just cause trouble itself; it messes up your entire gum ecosystem, making it easier for other harmful bacteria to thrive and harder for your body’s defenses to work. It’s like the bacteria that paves the way for the rest of the wrecking crew.
I remember a patient—let’s call him Mark—who came in frustrated. He brushed and flossed religiously but still had bleeding gums and a persistent bad taste. His test came back positive for high levels of P. gingivalis. He felt like he was failing at basic hygiene. That’s the sneaky part. Sometimes, good home care alone isn’t enough once this particular bug has established a stronghold. That’s when a targeted Porphyromonas gingivalis treatment plan becomes essential.
How Do You Even Know You Have It? Diagnosis Comes First.
You can’t treat what you haven’t identified. Guessing based on symptoms is a bad game. Bleeding gums (gingivitis) can be caused by many things. The presence of P. gingivalis specifically points toward active or looming periodontitis.
Your dentist or periodontist has a few tools:
- The Clinical Exam: The foundation. They’ll use a probe to measure the pockets (spaces) between your gums and teeth. Deeper pockets (over 4mm) often indicate bone loss and are prime real estate for bacteria like P. gingivalis to hide.
- Bacterial DNA Testing: This is the gold standard for pinpointing the culprit. A tiny sample of plaque is taken from your gum pockets and sent to a lab. The test, like those from companies like OralDNA Labs, doesn’t just confirm if P. gingivalis is present; it tells you how much is there. This is huge. It moves treatment from a generic “you have gum disease” to a specific “you have a high load of this aggressive pathogen.”
- Traditional Culture Tests: Less common now, but still used in some research or complex cases.
Getting tested might feel like an extra step, but it demystifies the problem. For Mark, seeing the lab report was a turning point. It wasn’t his fault; it was a specific bacterial infection that needed a specific strategy.
The Core of Porphyromonas Gingivalis Treatment: Professional Intervention
This is the non-negotiable part. P. gingivalis burrows deep into gum pockets and forms a tough, protective layer called biofilm (plaque’s more advanced, evil cousin). You can’t brush or floss it away from down there. The goal of professional treatment is to disrupt this biofilm and physically remove the bacterial colonies and the calculus (tartar) they live on.
A quick reality check: No mouthwash, magic toothpaste, or dietary supplement you can buy online will cure a significant P. gingivalis infection on its own. They can be helpful adjuncts (supporting players), but the star of the show is always professional mechanical cleaning. Anyone telling you otherwise is selling something.
Scaling and Root Planing (SRP): The Deep Clean
This is the first-line, cornerstone Porphyromonas gingivalis treatment. You might know it as a “deep cleaning.” It’s usually done in sections over two or more visits.
- Scaling: Using specialized ultrasonic and hand instruments, the hygienist or dentist removes plaque and tartar from above and below the gumline, all the way down to the bottom of the pockets.
- Root Planing: This is the critical part. The root surfaces of the teeth are smoothed out. Why? A rough root is a bacterial Airbnb. Smoothing it makes it harder for P. gingivalis and its friends to re-attach quickly.
Is it fun? Not really. It can be uncomfortable, and local anesthesia is often used. But the reduction in inflammation afterward is usually dramatic. For many people with mild to moderate periodontitis, SRP is enough to bring bacterial loads, including P. gingivalis, way down.
When SRP Isn't Enough: Surgical Options
If pockets remain deep after SRP, it means bacteria are still hiding in areas the instruments can’t reach. That’s when a periodontist might recommend surgery. The idea is to get direct visual access to clean the roots thoroughly and sometimes even reshape the bone and gum tissue to eliminate the pockets.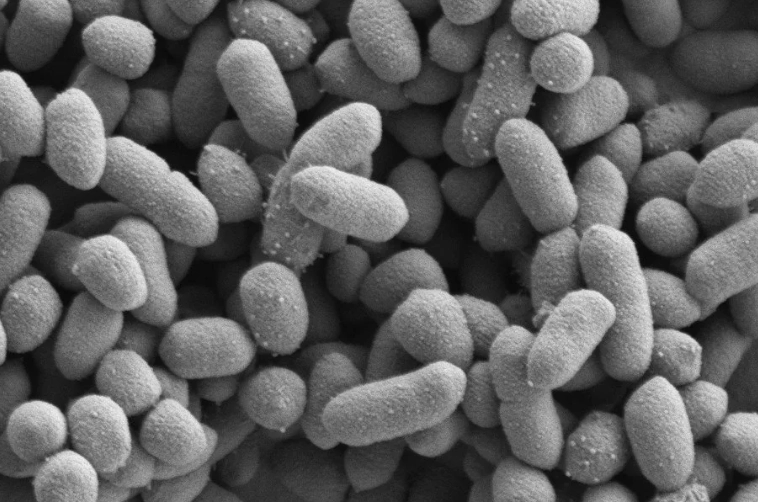
Types include flap surgery, bone grafts, and guided tissue regeneration. These are more invasive, but for advanced cases, they are the most effective way to save teeth and create an environment where bacteria can’t easily return.
The Antibiotics Question: To Use or Not to Use?
This is a big topic. Antibiotics don’t replace SRP; they can be used alongside it. The biofilm protects the bacteria, so you must break it up with SRP first for antibiotics to be truly effective.
Systemic antibiotics (pills) were used more commonly in the past. Now, the trend is toward local delivery antimicrobials. These are tiny gels, chips, or fibers containing antibiotics like doxycycline or minocycline that are placed directly into the gum pockets after SRP. They release medication right at the site of infection over a period of days.
Local vs. Systemic Antibiotics for P. gingivalis:
| Method | Pros | Cons |
|---|---|---|
| Local Delivery (Gel/Chip) | High concentration at the site; minimal body-wide side effects; no risk of gut microbiome disruption or systemic resistance. | Only treats the specific pockets it's placed in; requires precise application by a professional. |
| Systemic (Oral Pills) | Treats the entire mouth, including areas not yet showing disease; can address bacteria that may have traveled elsewhere. | Higher risk of side effects (nausea, yeast infections); contributes to broader antibiotic resistance; disrupts gut bacteria. |
The decision is highly individual. Factors include the severity of your infection, your medical history, and whether you’ve had SRP before with poor results. A study published by the American Academy of Periodontology often reviews these protocols, and their guidelines are what most specialists follow. The takeaway? Don’t demand antibiotics. Have a detailed chat with your periodontist about whether they are a necessary part of your Porphyromonas gingivalis treatment plan.
Your Role At Home: The Treatment Doesn't End at the Dentist's Door
Professional treatment resets the clock. Your daily routine determines if it stays reset. This is where you have massive control.
The Non-Negotiable Basics:
- Brushing: Twice daily with a soft-bristled brush. Technique matters—angle the bristles toward the gumline. Electric toothbrushes (especially sonic ones) get a strong recommendation from me for their consistency.
- Flossing/Interdental Cleaning: Once a day. If you hate string floss, try water flossers or interdental brushes. The goal is to disrupt biofilm between teeth, the other favorite hiding spot. A water flosser on a low-to-medium setting can be particularly good at flushing out debris from pockets.
Targeted Adjuncts That Can Help:
After SRP, your dentist might recommend specific products to help manage the bacterial load as you heal.
- Antimicrobial Mouthwashes: Chlorhexidine gluconate is the heavy hitter, often prescribed for short-term use (e.g., 2 weeks) post-treatment. It’s very effective but can stain teeth and alter taste. Cetylpyridinium chloride (CPC) mouthwashes are a good over-the-counter option for longer-term maintenance.
- Probiotics for Oral Health: This is an emerging area. The theory is that introducing beneficial bacteria (like specific strains of L. reuteri or L. brevis) can help crowd out the harmful ones. The evidence isn’t as rock-solid as for SRP, but some patients report great results. I view them as a potential supportive tool, not a primary treatment.
- Dietary Considerations: P. gingivalis thrives on inflammation. An anti-inflammatory diet (rich in omega-3s, antioxidants, low in processed sugars and refined carbs) supports your body’s overall healing response. It’s not a direct kill strategy, but it strengthens your defenses.
Think of your home care as the daily security detail for your gums. The professional treatment kicked out the squatters. Your job is to make sure they can’t easily move back in.
What Does Success Look Like? Monitoring and Maintenance
Treating P. gingivalis isn’t a one-and-done event. It’s a management plan. After active treatment (like SRP), you enter a critical phase called periodontal maintenance.
- More Frequent Cleanings: Forget the “every six months” rule. For periodontal patients, cleanings every 3-4 months are standard. This frequent disruption prevents the bacterial biofilm from maturing enough to cause damage again.
- Re-testing: About 3-6 months after treatment, a follow-up bacterial DNA test can be incredibly motivating. Seeing a “high” load turn into a “low” or “not detected” result is concrete proof the Porphyromonas gingivalis treatment is working.
- Pocket Re-checking: Your dentist will re-measure your gum pockets to see if they have reduced in depth—a sign of healing.
Success means no bleeding, reduced pocket depths, stable bone levels on X-rays, and low bacterial counts. It means controlling the infection, not necessarily eradicating every single bacterium forever (which may be impossible). The goal is to reduce it to a level your immune system can handle without destruction.
Common Questions People Are Afraid to Ask

Putting It All Together: A Realistic Action Plan
Feeling overwhelmed? Don’t be. Here’s a straightforward path.
Step 1: Get a Proper Diagnosis. See a dentist or periodontist. Ask about bacterial testing if you have signs of gum disease (bleeding, puffiness, bad breath, recession). Don’t just guess.
Step 2: Commit to the Professional Cleanings. If SRP is recommended, schedule it. This is the most important step in your Porphyromonas gingivalis treatment journey. Discuss antibiotic options (local vs. systemic) with your provider.
Step 3: Upgrade Your Home Game. Get an electric toothbrush, figure out an interdental cleaning tool you’ll actually use (floss, picks, water flosser), and ask your hygienist for prescription or recommended mouthwash for the short term.
Step 4: Embrace the Maintenance Schedule. Book your 3-4 month periodontal maintenance appointments before you even leave the office. Put them in your calendar as non-negotiable.
Step 5: Consider the Bigger Picture. Look at your diet, manage stress (it impacts inflammation), and if you smoke, please get help to quit. Smoking is arguably the single biggest risk factor for aggressive periodontitis and makes Porphyromonas gingivalis treatment much less effective.
Look, dealing with P. gingivalis is a pain. It really is. It’s expensive, time-consuming, and sometimes uncomfortable. But you know what’s worse? Losing teeth. The bone loss, the infections, the dentures or implants down the road. I’ve seen patients who put it off until it was too late, and the regret is real.
The path to beating this bug is clear, proven, and entirely doable. It’s a partnership between you and your dental team. Start the conversation today.