What’s Inside
- What a Periapical Abscess Really Is (And Why It's a Big Deal)
- Why a Regular Dental X-Ray Often Isn't Enough
- CBCT: The 3D Superpower for Dental Diagnosis
- Comparing Your Imaging Options: A Clear-Cut Table
- The Radiation Question: Should You Be Worried?
- What to Expect During the Scan: A Step-by-Step Walkthrough
- From Scan to Plan: How the Results Guide Your Treatment
- Common Questions About Periapical Abscess CT Scans
Let's talk about tooth pain. Not the little ache you get from a bit of cold ice cream, but the deep, throbbing kind that makes your whole jaw feel like it's pounding. The kind where you know something is seriously wrong. If you've been told you might have a periapical abscess (that's a nasty infection at the very tip of your tooth's root), and your dentist or endodontist is mentioning something about a CT scan, you're probably sitting with a mix of relief and new questions.
Relief because you're getting answers. Questions because, well, what exactly is a periapical abscess CT scan, and why do you need one? Isn't a regular dental X-ray enough?
I remember a friend who went through this. He had a root canal years ago, and out of the blue, his cheek started to swell. His regular dentist took an X-ray, saw a dark shadow, and said "possible infection." But it was only when he saw a specialist who ordered a CT scan for the periapical abscess that they saw the full picture—the infection had actually eaten a tiny tunnel through his jawbone. An X-ray just couldn't show that detail. That scan changed his entire treatment plan.
That's what we're diving into today. This isn't just medical jargon. It's about understanding the tool that can make the difference between a straightforward treatment and unexpected complications.
In a Nutshell
A periapical abscess CT (Computed Tomography) scan is a special 3D X-ray that gives dentists and endodontists a super-detailed, cross-sectional view of your tooth, its roots, the surrounding bone, and nearby critical structures like nerves and sinuses. It's the gold standard for complex dental infections because it reveals what traditional 2D X-rays hide.
What a Periapical Abscess Really Is (And Why It's a Big Deal)
First things first, let's get clear on the enemy. A periapical abscess isn't a surface-level problem. It starts inside your tooth.
Think of your tooth like a tiny castle. The hard enamel is the outer wall. Inside is the pulp chamber—the castle's living quarters, full of nerves and blood vessels. The roots are the castle's foundations, buried in your jawbone. If bacteria breach the walls (through a deep cavity, a crack, or an old filling), they invade the pulp. The immune system fights back, and that battle creates pus. That pus has nowhere to go, so it builds up at the very tip (apex) of the root, in the bone. That's your abscess.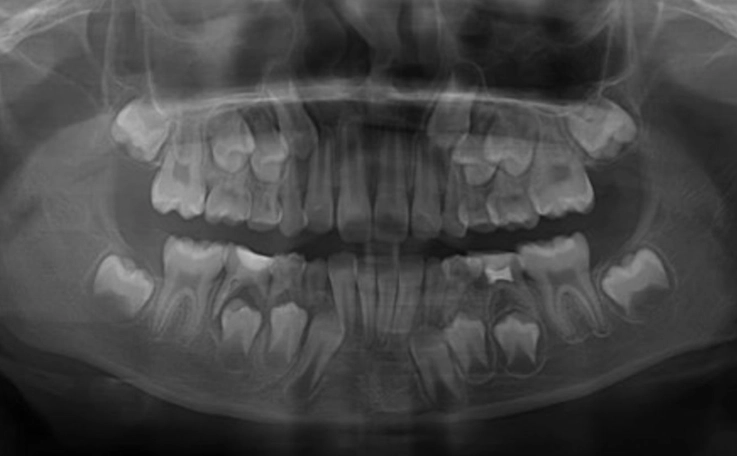
And it's not just sitting there. It's actively destroying bone. It's looking for an escape route, which can lead to swelling in your gums or face. Left unchecked, it can become a serious health risk. So diagnosing its exact size, shape, and path is critical.
Why a Regular Dental X-Ray Often Isn't Enough
Your dentist's 2D X-ray is a fantastic first tool. It's cheap, fast, and shows a lot. It can often show a dark, rounded area at the root tip, suggesting an abscess. But it has a major flaw: it compresses a complex 3D structure into a flat image.
Imagine taking a photo of a tree from just one side. You see the trunk and some branches, but you have no idea how deep the roots go, or if there's a beehive hidden around the back. That's the limitation.
Here’s what a standard X-ray might miss completely:
- The true size and shape of the bone destruction. Is it a small crater or a spreading cave?
- If the infection has perforated the bone wall.
- The exact number and curvature of tooth roots (some teeth have crazy, hooked roots).
- The precise relationship of the abscess to your maxillary sinus (above upper teeth) or the inferior alveolar nerve canal (running under lower teeth). Hitting these during treatment is a big deal.
- Additional, smaller abscesses or "accessory" canals that are infected.
- Fractures in the tooth root itself.
This is where the periapical abscess CT scan, specifically a CBCT (Cone Beam CT) designed for dentistry, becomes the game-changer.
CBCT: The 3D Superpower for Dental Diagnosis
When doctors talk about a dental CT, they're almost always referring to Cone Beam Computed Tomography. It's different from the big donut-shaped hospital CT scanner. A CBCT machine is smaller, often just rotates around your head once, and uses a cone-shaped X-ray beam to capture hundreds of images from different angles. A computer then stitches these into a breathtakingly detailed 3D model of your jaw.
You can literally scroll through slice-by-slice views of your jawbone, like slicing a loaf of bread and looking at each slice. You can view it from the front, the side, from above. You can measure distances to the millimeter. For planning treatment of a periapical abscess, this is invaluable intelligence.
What Your Doctor Sees in Your Periapical Abscess CT Scan
Let's break down the specific things your endodontist is hunting for when they analyze your scan. It's more than just "yep, there's an infection."
- Lesion Characterization: Is the boundary of the abscess well-defined (suggesting a slower, chronic process) or fuzzy and spreading (suggesting an aggressive, acute infection)? This influences treatment urgency.
- Bone Loss Dimensions: The exact height, width, and depth of the bone destroyed. This is crucial for prognosis—can the bone heal back after treatment?
- Anatomical Relationships: This is the big one. The scan maps exactly how close the abscess and tooth roots are to vital neighbors. For upper back teeth, how much bone is left between the root tip and the sinus floor? For lower teeth, is the abscess or root tip actually touching the nerve canal? The American Association of Endodontists (AAE) has clear guidelines on using CBCT for this precise mapping, which you can read about in their Guide to Clinical Endodontics.
- Root Canal Anatomy: Surprise extra canals, severe curves, or calcified (blocked) canals are all clearly visible. No more guesswork during the root canal procedure.
- Root Fractures: A vertical crack in the root is often a death sentence for a tooth. 2D X-rays miss most of them. A CT scan can frequently detect these fractures, saving you from a doomed treatment.

Comparing Your Imaging Options: A Clear-Cut Table
Let's put it all side-by-side. This table shows why a periapical abscess CT is reserved for specific, complex situations.
| Imaging Type | What It Shows (For Abscess) | Key Advantages | Key Limitations | Best Used For |
|---|---|---|---|---|
| Periapical X-ray | 2D view of 2-3 teeth, bone level, obvious large abscess. | Low cost, low radiation, readily available, good for initial detection. | Compression of anatomy, no 3D data, can miss size, shape, and relationships. | Initial screening, monitoring healing post-treatment. |
| Panoramic X-ray | Broad 2D view of entire jaw, teeth, sinuses, jaw joints. | Great for big-picture view, spotting other issues, low-ish radiation. | Blurry detail, distortion, still no 3D information. Poor for fine abscess anatomy. | Initial comprehensive exam, evaluating wisdom teeth, jaw fractures. |
| Cone Beam CT (CBCT) | 3D, detailed, slice-by-slice view of bone, tooth roots, abscess shape, sinus/nerve proximity. | Unmatched detail for complex anatomy. Essential for surgical planning. Reduces surprises. | Higher cost, higher radiation than X-rays (but lower than medical CT), not needed for simple cases. | Complex abscesses, re-treatment cases, suspected fractures, pre-surgical planning (apicoectomy). |
See the difference? The CBCT is the specialist's tool. It's not for every toothache. But when the situation is murky or high-risk, it provides clarity that nothing else can.
The Radiation Question: Should You Be Worried?
This is the elephant in the room. "CT" and "radiation" understandably make people nervous. Let's talk numbers and context, because fear often comes from the unknown.
A dental CBCT scan uses more radiation than a single small dental X-ray. That's a fact. But the key is that it uses significantly less radiation than a medical CT scan of your head you'd get in a hospital. Furthermore, the field of view is usually very targeted—just a few teeth, not your whole head.
Here’s some perspective. Radiation exposure is measured in microsieverts (μSv).
- A single dental periapical X-ray: about 5 μSv.
- A dental CBCT (small volume): between 20 to 100 μSv, depending on the machine and settings.
- A medical head CT: around 2,000 μSv.
- Natural background radiation you get from just living on Earth for one year: about 3,100 μSv.
So, a targeted dental CBCT exposes you to far less than you get from nature annually. The principle of ALARA (As Low As Reasonably Achievable) is a core tenet in radiology. Reputable clinics use this. They won't recommend a periapical abscess CT unless the potential diagnostic benefit clearly outweighs the minimal risk. The American Dental Association's Council on Scientific Affairs provides guidance on this justification process, which you can explore here.
A Quick But Important Note
Always tell your dentist if you are or might be pregnant. While the radiation dose to the abdomen from a dental CBCT is negligible, extra precautions are always taken, and non-urgent imaging is usually postponed. This is a standard, non-negotiable safety protocol.
What to Expect During the Scan: A Step-by-Step Walkthrough
Knowing what will happen can take the edge off. Here’s the typical process:
1. The Setup: You'll be led into a room with the CBCT machine. It looks a bit like a large, futuristic camera on a stand. You'll be asked to remove any metal from your head/neck (earrings, glasses, hairpins, removable dental work). You'll usually stand or sit, resting your chin on a support.
2. Positioning: The technician will adjust the machine so the area of interest is centered. They might use laser guides. They'll give you instructions like "bite gently on this plastic tab" or "keep your tongue against the roof of your mouth." Staying still is key.
3. The Scan: The machine's arm will rotate around your head in a slow, smooth arc—it takes between 10 to 40 seconds, depending on the machine. You'll hear a faint whirring or buzzing. That's it. No pain, no discomfort. You're alone in the room, but the technician can see and hear you.
4. Aftermath: That's literally it. You can go about your day immediately. No side effects. The images are digitally processed and sent to your specialist for analysis.
The whole appointment, from walking in to walking out, is often under 15 minutes. The actual scan time is the shortest part.
From Scan to Plan: How the Results Guide Your Treatment
So you've had the CT scan for your periapical abscess. What next? Your endodontist will sit down with you and go through the images. They might show you on a screen, pointing out the abscess, the roots, the nerve canal.
This information directly dictates the path forward:
Scenario A: A Straightforward (but now well-informed) Root Canal. The scan confirms the anatomy is manageable, the abscess is contained, and vital structures are at a safe distance. The root canal procedure proceeds with a detailed roadmap, increasing the chance of a complete clean-out and success.
Scenario B: A Complex Re-treatment. The scan reveals a missed canal, a severe curve, or a perforation from a previous treatment. The endodontist now knows exactly what challenges to expect and can use specialized tools and techniques from the start.
Scenario C: The Need for Apicoectomy (Root-End Surgery). Sometimes, a traditional root canal from the top of the tooth isn't possible or has failed. The scan is essential for planning this minor surgical procedure. It shows the surgeon exactly where to make a small incision in the gum, how much bone to remove to reach the root tip, and how to remove the abscess and infected root tip without damaging the nerve or sinus. It turns a blind procedure into a precise one.
Scenario D: The Hard Truth—Tooth Extraction. If the scan reveals a vertical root fracture, or that the bone loss is so severe the tooth has no support left, or that the infection is dangerously close to critical structures in an inoperable way, extraction might be the only safe option. It's a tough call, but a periapical abscess CT scan provides the evidence to make that call confidently, preventing you from undergoing costly, painful, and ultimately futile treatment.
Questions to Ask Your Doctor After the Scan
Don't be shy. This is your health. Good questions include: "Can you show me the abscess on the image?" "How close is it to the nerve/sinus?" "Based on this, what is the success rate for saving my tooth?" "Are there any unexpected findings?" A good specialist will welcome these questions.
Common Questions About Periapical Abscess CT Scans
Is a CT scan always necessary for a tooth abscess?
Absolutely not. For many clear-cut, first-time abscesses on front teeth with simple anatomy, a regular X-ray is sufficient. The American Association of Endodontists recommends CBCT when the benefits of the 3D information outweigh the risks, typically in complex cases like re-treatment, suspected fractures, unusual anatomy, or before surgery. It's a targeted tool, not a routine one.
How much does a dental CT scan cost?
This varies wildly by region and practice. In the US, you might see a range from $200 to $600. It's often an out-of-pocket expense, as dental insurance can be spotty in covering advanced imaging. Always check with your insurance provider and your dental office for an estimate beforehand. It's a frustrating part of the process, but knowing avoids a nasty surprise bill.
Can I get a copy of my CT scan?
Yes, you should be able to. You have a right to your medical/dental records. Ask the office for a digital copy (usually on a CD or via a secure download link). This is especially useful if you seek a second opinion. The file format is usually DICOM, which any dental specialist can open in their software.
What's the difference between a medical CT and a dental CBCT for an abscess?
Medical CT scanners use a fan-shaped beam and a rotating detector, capturing multiple slices with higher overall radiation dose but excellent soft tissue detail. Dental CBCT uses a cone-shaped beam and a single rotation, capturing a volume of data with lower radiation but much higher spatial resolution for bone and teeth. For purely dental bone and tooth issues, CBCT is the superior, safer tool. For evaluating deep neck space infections from a dental abscess (a rare but serious complication), a medical CT or MRI might be needed.
How long does it take to get results?
The images are available almost instantly. The analysis and interpretation by your specialist take time. Often, they will review them shortly after the scan and discuss findings with you in the same appointment or a follow-up consultation soon after.
Look, dental problems are stressful enough without the confusion of medical technology. My goal here was to pull back the curtain on the periapical abscess CT scan. It's not magic, and it's not something to be automatically feared. It's a powerful, precise lens.
It gives your doctor the clarity to make the best possible decision for your tooth.
And in the end, that's what we all want—the best shot at saving our natural teeth and getting out of pain for good. If your specialist recommends one, see it not as an extra step, but as the step that could make all the difference.
Leave a Reply