You know the feeling. You wake up with a dull ache in your temples, a tightness in your jaw that feels like you’ve been chewing gravel all night. Or maybe your partner has nudged you awake again, complaining about the grating sound. Bruxism – the medical term for teeth grinding and jaw clenching – is a frustratingly common problem. But when you search for bruxism causes, you’re often met with a one-word answer: stress.
That’s only part of the story, and frankly, it’s an oversimplification that leaves a lot of people confused. If stress were the only cause, managing it would be the universal cure, and we know it’s not that simple.
After years of seeing patients and digging into the research, I’ve found the real picture is more like a puzzle. For most people, it’s not one single cause but a combination of factors that tip the scales. Sometimes it’s a physical issue your body is trying to correct. Other times, it’s a side effect of how your brain sleeps. Let’s put that puzzle together.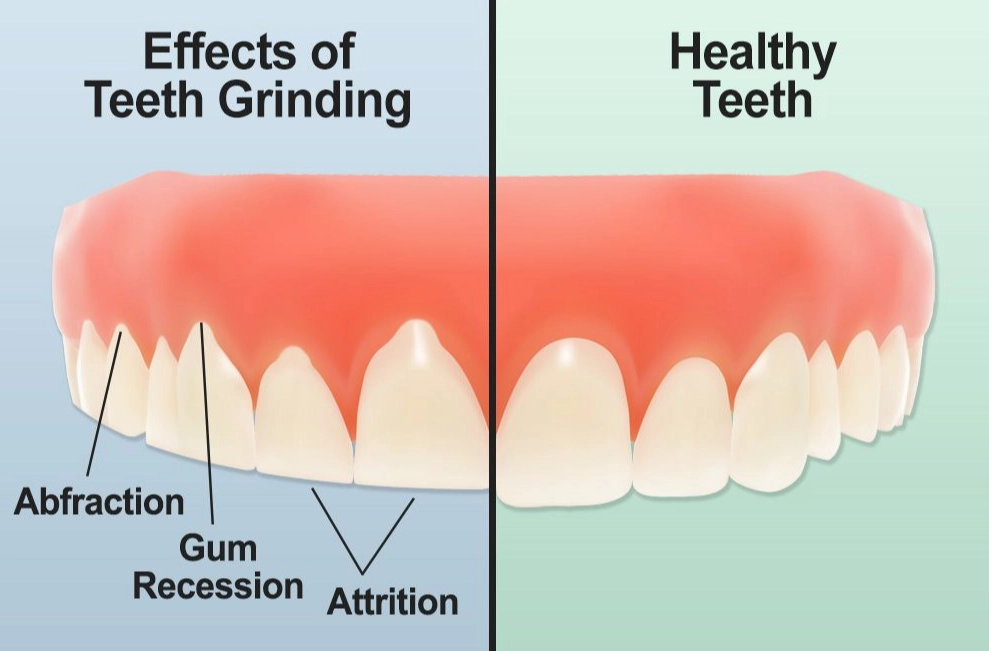
What’s Inside This Guide
The Sleep Connection: More Than Just a Bad Dream
This is the big one for nighttime grinders, and it’s where the science gets fascinating. Sleep bruxism is now classified as a sleep-related movement disorder, often happening during micro-arousals from sleep.
Think of your sleep cycle like a road. Bruxism tends to happen at the potholes – those brief, partial awakenings you don’t even remember.
Sleep Apnea’s Role: The link here is strong. Studies referenced by the American Academy of Sleep Medicine show a high correlation between obstructive sleep apnea (OSA) and bruxism. The theory? When your airway starts to collapse and your breathing is interrupted, your brain triggers a micro-arousal. As part of that arousal response, it may also activate the jaw muscles, causing a grinding or clenching episode as a way to possibly help open the airway. It’s your body’s clumsy, destructive attempt to keep you breathing.
If you snore loudly, gasp for air at night, or have crushing daytime fatigue, this connection needs to be your first stop. Treating the apnea with a CPAP machine or oral appliance can, for many, dramatically reduce or even stop the grinding.
Other Sleep Disorders: It’s not just apnea. Insomnia, restless leg syndrome, and even talking in your sleep can be associated with increased sleep fragmentation and higher rates of bruxism.
Key Takeaway: Don’t just tell your dentist you grind your teeth. Tell your doctor you’re exhausted. A sleep study might reveal the root cause that a night guard can only protect against.
The Physical Triggers Your Dentist Might Spot
Sometimes, the cause is right there in your mouth. Your jaw muscles are incredibly powerful, and they’re always seeking a position of comfort and stability.
Malocclusion (The “Bad Bite”)
If your teeth don’t fit together properly—maybe a tooth is tilted, a crown is a bit too high, or your overall bite is misaligned—your muscles can go into overdrive. They’ll grind and clench subconsciously, trying to wear down the interference and find a stable spot. This is a classic, yet often debated, physical cause.
Some dentists see it as primary; others think it’s a minor player unless the misalignment is severe. In my experience, it’s particularly relevant if your grinding seems focused on one specific area.
TMJ Disorders (TMD)
Which came first, the grinding or the joint disorder? It’s a chicken-and-egg situation. Bruxism can cause or worsen TMD by overworking the joint. Conversely, pain and dysfunction in the TMJ can cause the muscles to spasm and clench in response. They become intertwined problems.
Posture and Ergonomics
Here’s one most people miss. Spend 8 hours a day with your head jutting forward over a computer? That forward head posture places immense strain on the muscles that close your jaw (the masseters and temporalis). They’re already in a shortened, stressed state. Clenching at night can be a continuation of that pattern.
Lifestyle & Medication: The Hidden Contributors
What you consume can directly wire your nervous system for grinding.
| Factor | How It Contributes | Notes |
|---|---|---|
| Caffeine & Stimulants | Increases overall muscle activity and arousal, making it harder for your nervous system to fully relax during sleep. | That 4 PM coffee might be fueling your midnight grind. |
| Alcohol | Disrupts sleep architecture, leading to more fragmented, lower-quality sleep and increased arousal episodes. | While it may help you fall asleep, it worsens sleep quality later in the night. |
| Smoking/Nicotine | Nicotine is a stimulant. Smokers also have higher rates of sleep apnea. | A double whammy for bruxism risk. |
| Certain Medications | Some SSRIs (a class of antidepressants like fluoxetine or sertraline) and SNRIs list bruxism as a known side effect. | Never stop medication without consulting your doctor. A dosage adjustment or switch may help. |
| Recreational Drugs | Stimulants like MDMA, cocaine, and methamphetamine are notorious for causing severe bruxism. | The effects can be intense and cause rapid dental damage. |
Stress & Anxiety: The Fuel, Not Always the Fire
Okay, let’s talk about it. Yes, stress and anxiety are major, major players. But I want to refine this idea.
For awake bruxism (clenching during the day), stress is often the direct trigger. It’s a physical manifestation of tension, concentration, or frustration. You might catch yourself doing it at your desk, in traffic, or while reading a tense email.
For sleep bruxism, stress acts more like an amplifier. It doesn’t necessarily create the grinding mechanism itself (which is often tied to sleep arousal), but it heightens your overall nervous system arousal, making those micro-arousals more frequent and intense. It pours gasoline on the existing fire.
Furthermore, the type of stress matters. It’s not just big life events. It’s chronic, low-grade stress—the constant buzz of deadlines, financial worry, or caregiving—that keeps your nervous system in a perpetual state of “high alert,” priming you for bruxism.
Perfectionists and people with high anxiety traits are often more prone. Their baseline muscle tone is simply higher.
What Now? Steps to Take After Identifying Potential Causes
So you see yourself in a few of these categories. What’s the next move? This isn’t about quick fixes, but a diagnostic journey.
1. Start a Symptom Journal. For two weeks, note: Jaw pain level (morning/evening), headache frequency, perceived stress level, caffeine/alcohol intake, and sleep quality. Patterns will emerge.
2. Book a Dental Check-Up. Go beyond the cleaning. Tell your dentist you suspect bruxism. They can check for wear facets on your teeth, tongue scalloping (indentations from pressing against teeth), and hypertrophied jaw muscles. They can also assess your bite and TMJ.
3. Talk to Your Primary Care Physician. Discuss your sleep quality, fatigue levels, and medication list. Mention the bruxism. This is the step to get a referral for a sleep study if apnea is suspected.
4. The Night Guard Conversation. A custom-fit occlusal guard from your dentist is the gold standard for protection. It won’t stop the causes, but it will save your teeth from destruction while you figure them out. Avoid cheap boil-and-bite guards—they can worsen clenching and misalign your bite.
5. Build Your Management Toolkit. Based on your suspected causes: - For sleep/suspected apnea: Pursue a sleep study. - For stress/anxiety: Cognitive Behavioral Therapy (CBT) has good evidence for bruxism. Explore mindfulness, meditation, or regular aerobic exercise. - For physical/postural: Consider physical therapy focused on the head, neck, and jaw. Assess your workstation ergonomics. - For lifestyle: Gradually cut back on afternoon caffeine, reduce evening alcohol, and aim for consistent sleep hygiene.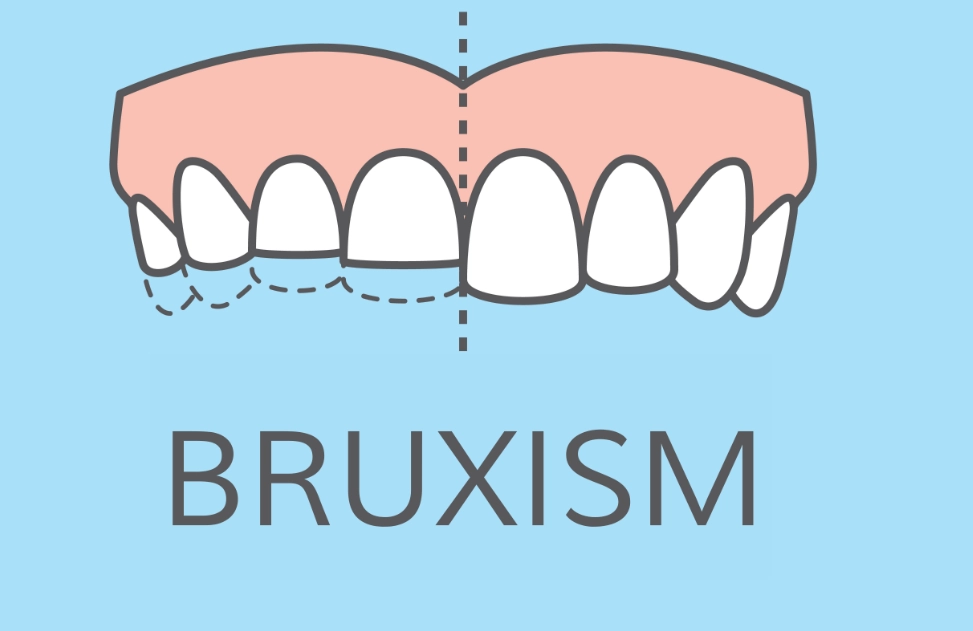
Your Bruxism Questions, Answered
 My dentist said my bite is off. Could that really be the main cause of my bruxism?
My dentist said my bite is off. Could that really be the main cause of my bruxism?