Quick Navigation
- Why a Broken-Off Tooth is a Tricky Customer
- The Step-by-Step: From Panic to Procedure
- What About Pain? Let's Talk Real Expectations
- Recovery Roadmap: What Normal Looks Like
- The Big Question: To Pull or Not to Pull? (Exploring Alternatives)
- Cost Factors: What Makes the Price Tag Swing?
- Your Burning Questions, Answered
- Final Thoughts: Don't Let Fear Decide
Let's get straight to the point, because if you're reading this, you're probably in some discomfort or worried about a tooth that's given up the ghost right at the gumline. It's a frustrating situation. One minute you're chewing, the next you're spitting out a piece of your molar. The rest seems to have vanished below the pink tissue, leaving you wondering what on earth a dentist can even do with that.
The short, direct answer is yes, a dentist can absolutely pull a tooth that is broken off at the gum line. It's one of the more common dental predicaments they deal with. But—and this is a big but—it's rarely as simple as the classic "yank it out" image you might have. Calling it a "pull" is almost an oversimplification. When there's no crown to grip, the game changes entirely. The process becomes more of a precision surgical procedure than a simple extraction.
I remember a friend who had a molar break at the gum line. He kept putting off the dentist, convinced it would be a horrific, impossible surgery. He lived on one side of his mouth for months. When he finally went, his dentist had it out in under 30 minutes. The relief on his face wasn't just from the pain ending; it was from the anxiety melting away. The unknown is often worse than the procedure itself.
This guide is here to strip away that unknown. We're going to walk through exactly what happens when you need a tooth broken at the gum line extracted. Not just the "can they," but the how, the why, the how long, and the what next. We'll look at the tools, the techniques, the recovery, and the all-important question: is pulling it even the best option, or should you try to save it?
Why a Broken-Off Tooth is a Tricky Customer
You can't just grab what you can't see. That's the core of the issue. A standard extraction uses forceps that clamp onto the visible part of the tooth (the crown) for leverage. When the break is flush with or below the gum, that handle is gone. The dentist is now working blind on a target submerged in bone and tissue.
The tooth root is still there, anchored in your jawbone by the periodontal ligament. It might be intact, or it might be fractured itself. There could be decay going deep down the root. The bone around it might be weak. All of these factors turn a routine job into a puzzle. The goal shifts from pulling to carefully removing the root structure while preserving as much surrounding bone and gum as possible. This is crucial for future dental work, like an implant.
Frankly, this is where experience matters. A general dentist comfortable with surgery can handle many cases, but for really complex breaks, deep fractures, or teeth curved like corkscrews, they might refer you to an oral surgeon. It's not an admission of failure; it's them making sure you get the right specialist for your specific problem.
The Step-by-Step: From Panic to Procedure
Step 1: The Diagnosis – Seeing the Unseen
You can't fix what you can't diagnose. Before anyone even thinks about tools, your dentist needs a clear map of the battlefield. This almost always means an X-ray, and often a specific kind called a periapical X-ray or a panoramic X-ray.
Why is this so critical? The X-ray reveals the secrets below the surface:
- Root Shape and Number: Is it a single straight root? Multiple roots? Are they curved or hooked? Molars, especially, can have roots that look like they're hugging the bone for dear life.
- Root Condition: Is the root tip also fractured? Is there a crack running down its length?
- Bone Health: How much bone surrounds the root? Is there an infection (an abscess) at the tip showing up as a dark spot?
- Relationship to Neighbors: How close is it to the sinus cavity (upper teeth) or the nerve in your jaw (lower teeth)?
This visual intel lets the dentist plan the attack. They'll decide if it's a job for them or if an oral surgeon is the better call. They'll also have a frank conversation with you about the complexity, which directly influences the time, technique, and cost.
Step 2: The Techniques – How They Actually Get It Out
This is the meat of the question, "Can a dentist pull a tooth that is broken off at the gum line?" Here are the main methods, from least to most invasive.
The Simple (or Closed) Extraction – A Rare Win
If you're lucky, and I mean really lucky, a tiny fragment of tooth might still be visible or just under the gum, and the root is straight and short. In this best-case scenario, the dentist might gently lift the gum, use a special tool called an elevator to wedge between the root and bone, and work it loose enough to grip with forceps. But let's be real—for a true "broken off at the gum line" situation, this is the exception, not the rule.
The Surgical (or Open) Extraction – The Standard Playbook
This is the most common answer for extracting a tooth broken at the gum line. It's a minor surgery. Here's the play-by-play:
- Numbing Up: You'll get local anesthesia (like Novocain). For severe anxiety or complex cases, sedation (like nitrous oxide or IV sedation) is an option. You won't feel pain, just pressure.
- Accessing the Root: The dentist makes a small incision in the gum to flap it back, exposing the underlying bone and the top of the root.
- Bone Removal: Using a fine drill or hand instruments, a tiny amount of bone surrounding the root is carefully removed. This creates a channel to reach the tooth.
- Tooth Sectioning: Often, especially with multi-rooted teeth, the root is cut into pieces with the drill. Removing smaller sections is easier and causes less trauma than trying to remove one big, awkward shape.
- Elevation and Delivery: Those elevator tools are used again to gently loosen each root fragment. They might then use forceps or a different tool called a root tip pick to lift the pieces out.
- Cleanup and Closure: The socket is cleaned of any debris. Sometimes, if a lot of bone was removed or there was an infection, they might place a bone graft material to aid healing. The gum flap is then stitched back into place with dissolvable stitches.
The whole thing usually takes 30 to 60 minutes, depending on the tooth's stubbornness.
Minimally Invasive Techniques
Some dentists now use specialized kits designed for these tricky extractions. Tools like periotomes or physics forceps use controlled force or leverage to literally push the tooth out of its socket with minimal to no cutting of bone or gum. It's fantastic when it works—faster healing, less swelling. But it's not suitable for all cases, particularly those with severely curved roots or dense bone. It's worth asking your dentist if you're a candidate.
Extraction Technique Comparison
| Technique | Best For | Invasiveness | Typical Healing Time | Key Advantage |
|---|---|---|---|---|
| Simple/Closed | Visible tooth structure, straight roots | Low | 3-7 days | Quick, minimal trauma |
| Surgical/Open | Most broken-at-gumline cases, curved/fractured roots | Moderate-High | 7-14 days (initial) | Predictable, handles complexity |
| Minimally Invasive (e.g., Physics Forceps) | Selected cases with favorable anatomy | Very Low | 3-7 days | Preserves bone, faster recovery |
What About Pain? Let's Talk Real Expectations
The number one fear. During the procedure, the anesthesia ensures you don't feel sharp pain. You'll feel pushing, pressure, vibrations from the drill—sensations that can be weird and unsettling, but not painful. Communicate with your dentist. A raised finger is all it takes to get more numbing agent.
Afterwards is a different story. Once the numbness wears off (in 2-4 hours), you will have discomfort. Calling it "pain" depends on your tolerance and the complexity of the extraction. A straightforward surgical extraction might feel like a deep ache. A more involved one will hurt more. Your dentist will prescribe pain medication (often ibuprofen and sometimes something stronger) and give very specific aftercare instructions. The first 48 hours are the toughest, then it steadily improves.
Recovery Roadmap: What Normal Looks Like
Healing from extracting a tooth broken at the gum line follows a predictable path, but it's not always a smooth one.
- First 24 Hours: Bleeding (oozing) is normal. Bite firmly on the gauze. Swelling peaks. Stick to cool, soft foods (yogurt, pudding, smoothies). No spitting, sucking (through a straw), or smoking! These can dislodge the blood clot forming in the socket, leading to a painful condition called dry socket.
- Days 2-3: Swelling and bruising may be most noticeable. Transition to lukewarm, soft foods (mashed potatoes, scrambled eggs). Start gentle saltwater rinses (1/2 tsp salt in warm water) after 24 hours to keep the area clean.
- Days 4-7: Significant improvement. Discomfort should be manageable with over-the-counter meds. You can gradually reintroduce more solid foods as comfort allows.
- Week 2+: Stitches dissolve (if used). The gum tissue closes over. The underlying bone takes months to fully fill in, but you'll feel normal long before that.
Signs to call your dentist immediately: severe pain not relieved by medication, foul taste or pus, fever, or heavy bleeding. These could indicate an infection or dry socket.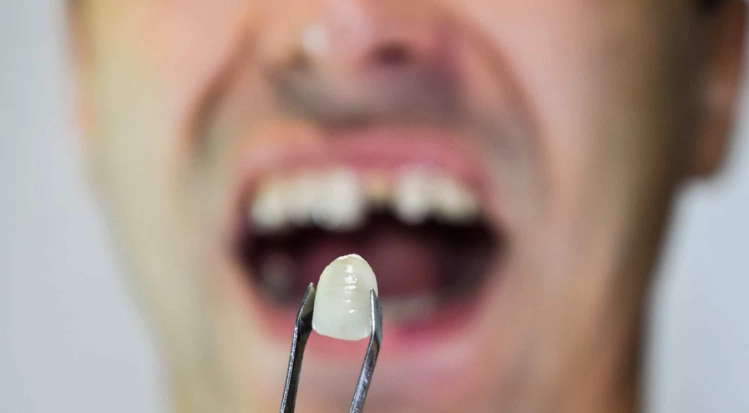
The Big Question: To Pull or Not to Pull? (Exploring Alternatives)
Just because a dentist can pull a tooth that is broken off at the gum line doesn't always mean they should. Extraction is a last resort. Saving your natural tooth is almost always preferable if it's structurally and financially feasible. Let's look at the contenders.
Root Canal Therapy + Post & Crown
If the break is clean and there's enough solid tooth structure below the gum line, this might be an option. The dentist (or an endodontist, a root canal specialist) removes the infected pulp from inside the root, cleans it, and fills it. Then, a metal or fiber "post" is cemented into the root, and a custom-made crown is built on top, extending down to cover the remaining tooth. It's a complex, expensive procedure, but it preserves your natural root and avoids an implant. Success depends heavily on the skill of the dentist and the quality of the remaining tooth. The American Association of Endodontists has great resources on when a tooth can be saved.
Dental Implant
This is often the gold standard replacement after an extraction. It involves placing a titanium screw in the jawbone where the root was, letting it fuse with the bone (osseointegration) over several months, then attaching a crown on top. The catch? It requires healthy bone and is a lengthy, costly process. But it's the closest thing to a natural tooth in function and feel. Sometimes, an implant can even be placed immediately after the extraction (immediate implant placement), but this is technique-sensitive. The American Academy of Implant Dentistry outlines the criteria.
Dental Bridge
An older but reliable option. The teeth on either side of the gap are crowned, and a false tooth is suspended between them. It's faster and cheaper than an implant but requires altering two healthy teeth. Not ideal if those neighboring teeth are pristine.
So, how do you decide? It's a cost-benefit-analysis conversation with your dentist. They should present you with all viable options, their long-term prognoses, and the costs. A root canal to save it might cost $1,500-$2,500. An extraction alone might be $200-$600. An extraction followed by an implant can run $3,000-$6,000. It's a big range.
Cost Factors: What Makes the Price Tag Swing?
There's no flat fee for extracting a tooth broken at the gum line. It depends on:
- Tooth Location: Molars are harder than front teeth.
- Complexity: Straight root vs. a tangled mess. Need for bone grafting?
- Provider: General dentist vs. oral surgeon (surgeons cost more).
- Geographic Location: NYC costs more than a small town.
- Anesthesia: Local vs. sedation (IV sedation adds significant cost).
- Insurance: Most dental plans cover extractions, but surgical ones may have different co-pays.
Always get a pre-treatment estimate. Ask for the procedure codes (like D7210 for surgical extraction) and call your insurance. The out-of-pocket for a surgical extraction can range from $75 to $450+ after insurance.
Your Burning Questions, Answered

Final Thoughts: Don't Let Fear Decide
A broken tooth at the gum line feels like a dental emergency, and in a way, it is. But it's a solvable problem. The technology and techniques are there. The answer to "can a dentist pull a tooth that is broken off at the gum line?" is a resounding yes, but the real story is in the nuance—the diagnosis, the surgical skill, and the aftercare.
Putting it off is the worst thing you can do. Decay spreads. Infections form. Bone loss occurs. What could have been a manageable extraction can turn into a much bigger ordeal.
My advice? Make the call. Get the X-ray. Have the conversation. Know your options. Whether it's a strategic extraction or a heroic effort to save the tooth, taking control of the situation is the first and most important step toward getting your smile—and your peace of mind—back.
It's not fun. Nobody looks forward to it. But the relief of having it handled, the pain gone, and a plan for the future in place is worth every moment of anxiety beforehand. Trust me on that.