So you've just had a periodontal scaling, sometimes called a deep cleaning. The numbness is starting to wear off, and you're probably sitting there thinking, "Okay, now what?" Let's be real, the procedure itself isn't exactly a day at the spa, and the uncertainty about what comes next can be the worst part. I've talked to countless patients in this exact spot, feeling a mix of relief that it's over and anxiety about the healing process.
Knowing what to expect after periodontal scaling is the key to a smooth recovery and, more importantly, to making sure all that effort (and investment) pays off for your long-term oral health. This isn't just about getting through a few days of soreness; it's about actively partnering in your gum healing. This guide will walk you through every stage, from the first few hours to the months ahead, cutting through the confusion with straight talk and practical advice.
The bottom line upfront: Your mouth has been through a significant therapeutic procedure. Discomfort, sensitivity, and minor bleeding are normal guests for a short while. Your job is to manage them gently and consistently. The goal is to let your gums reattach to now-clean tooth roots, shrinking those pockets and getting you off the path of gum disease.
The Immediate Aftermath: The First 24 Hours
The anesthesia is your friend, but it doesn't last forever. As it fades, usually within a few hours, you'll start to feel what's what. Here’s a breakdown of the most common sensations and how to handle them.
Sensations You'll Likely Feel
tenderness and Aching: This is the big one. Your gums have been worked on intensively. They are inflamed from the existing infection and now from the therapeutic trauma of cleaning. A dull, general ache across the treated quadrants is completely standard. It often feels like a bruise or a deep soreness.
Tooth Sensitivity: Oh boy, the sensitivity. This can be a real surprise for some people. Since plaque and tartar (calculus) that was insulating the roots has been removed, and because the gums are slightly lower, the root surfaces are now exposed to air, water, and temperature. Drinking room-temperature water might suddenly feel... noticeable. This is a classic sign of what to expect after periodontal scaling and root planing.
Minor Bleeding: A little pink in your saliva is normal. Your gums are healing. Think of it like a scrape on your knee that weeps a bit. It should subside significantly within the first day. Oozing or persistent bleeding is a different story, which we'll cover later.
weird Taste or Small: The antimicrobial rinses or medicaments used during the procedure can leave a medicinal taste. Also, as the healing process starts and tiny bits of old blood mix with saliva, you might notice a metallic taste. It passes.
Your Action Plan for Day One
- Pain Management: Take the over-the-counter pain reliever your dentist recommended (like ibuprofen or acetaminophen) before the numbness fully wears off. Staying ahead of the pain is easier than chasing it. I'm not a fan of suffering needlessly—pop that pill on schedule for the first day.
- The Diet Shift: Stick to soft, cool, and bland foods. Mashed potatoes, yogurt, smoothies (not too cold!), soup (let it cool), scrambled eggs. Avoid anything crunchy, spicy, acidic (like orange juice), or hot in temperature. That hot coffee can wait till tomorrow.
- Leave the Area Alone: Do not poke, prod, or explore the area with your tongue or finger. Do not rinse vigorously. Just let it be. Gentle is the mantra.
The First Week: The Healing Marathon
Days 2 through 7 are where the real healing kicks in. The initial soreness should gradually decrease. Swelling might peak around day 2 or 3 and then subside. Here’s a simple table to visualize a typical timeline for what to expect after periodontal scaling in week one:
| Day | Common Symptoms | Do's & Don'ts Focus |
|---|---|---|
| 1-2 | Peak soreness, sensitivity, minor bleeding. | Soft diet, gentle hygiene, pain meds as needed. |
| 3-4 | Soreness fading, sensitivity persists, gums may feel "tight" or itchy as they heal. | Introduce very gentle brushing in treated areas. Continue saltwater rinses. |
| 5-7 | Significant improvement. Most discomfort gone, sensitivity slowly improving. | Resume more normal (but still careful) brushing and flossing. Diet can slowly normalize. |
Mastering Your New Cleaning Routine
This is the most critical part of the entire process. The scaling removed the existing problem, but your daily routine prevents it from coming back. Your technique needs to adapt to your newly cleaned, more sensitive teeth.
Your At-Home Care Arsenal:
- Ultra-Soft Toothbrush: Toss your medium or hard brush. An ultra-soft brush is non-negotiable.
- Sensitivity Toothpaste: One with potassium nitrate or stannous fluoride. Use it consistently, not just when it hurts. It takes days to weeks to build up its protective effect.
- Interdental Brushes or Soft Picks: If your dentist recommended these for the spaces between your teeth, use them. They are often gentler and more effective than floss on tender gums and wider spaces.
- Antimicrobial Rinse: If prescribed (like chlorhexidine), use it exactly as directed. It's a powerful tool to control bacteria while you can't brush as effectively. Don't use it long-term without asking, as it can stain teeth.
- Warm Salt Water Rinse: The old classic. 1/2 teaspoon of salt in a cup of warm water. Gently swish after meals. It's soothing, reduces bacteria, and promotes healing. I recommend this to almost everyone.
Brushing technique is everything now. Use the soft brush at a 45-degree angle towards the gumline, using tiny, gentle, circular or vibrating motions. You're massaging and cleaning, not scrubbing a tile floor. If your gums are still tender, just focus on the chewing surfaces and the inner/outer surfaces away from the gumline for the first few days, then gradually work your way back to the gumline as comfort allows.
When to Sound the Alarm: Not Everything is "Normal"
Most recoveries are straightforward. But sometimes, your body sends up a red flag. Knowing the difference between standard healing and a potential problem is crucial. Don't just tough it out if you experience any of the following.
Contact Your Dentist or Periodontist Immediately If You Experience:
- Severe, Throbbing Pain that isn't touched by over-the-counter meds and gets worse after 2-3 days.
- Heavy or Persistent Bleeding that doesn't slow down when you apply gentle pressure with a clean gauze pad for 15-20 minutes.
- Significant Swelling that gets worse after day 3, especially if it's making it hard to open your mouth or breathe/swallow comfortably.
- Fever, Chills, or Pus coming from the gums. This indicates a possible infection.
- Numbness that persists well beyond the expected time for local anesthesia to wear off (e.g., still numb the next morning).
I had a patient once who thought increasing pain was just part of the deal. It turned out to be a small, trapped piece of food causing localized irritation. A quick visit for an irrigation solved it. The moral? When in doubt, call. It's better to have a 5-minute phone call for reassurance than to endure days of unnecessary discomfort or let a small issue become big.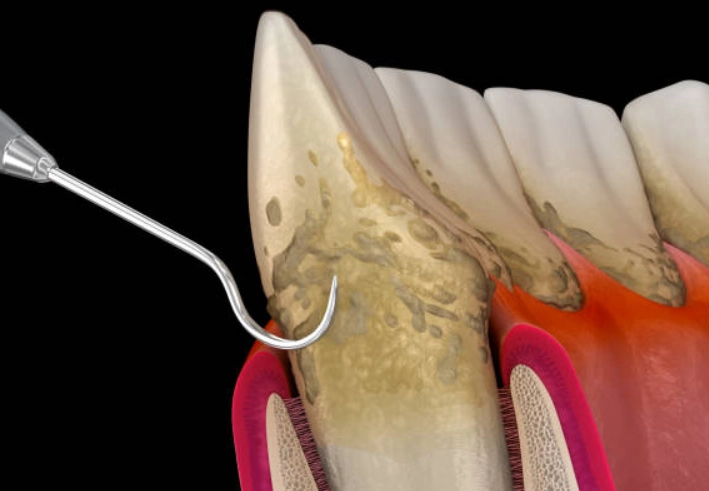
The Long Game: What Happens in the Weeks and Months After?
Your healing isn't done when the soreness stops. The biological goal—gum reattachment—is a slower process. Here's what to expect after periodontal scaling as time goes on.
Sensitivity: The Longest-Lasting Guest
This is the number one question I get at follow-ups. "When will the sensitivity go away?" For most, it improves dramatically within the first 2-4 weeks. For some, especially with deep pockets or significant root exposure, it can linger for a few months, gradually getting better. Consistent use of sensitivity toothpaste is your best defense. If it's really bothersome, talk to your dentist about in-office fluoride varnish or desensitizing treatments.
Follow-Up Appointments Are Non-Negotiable
That 4-6 week re-evaluation appointment isn't a suggestion. It's a critical check-up. The hygienist will gently probe your gums again to measure the pocket depths. This tells you and your dental team if the healing is on track. It's also a chance to review your home care technique and catch any areas you might be missing. According to the American Academy of Periodontology, this supportive periodontal therapy phase is essential for long-term success and preventing recurrence.
After that, you'll likely enter a more frequent maintenance schedule, often every 3-4 months instead of every 6. This isn't a punishment! It's a proactive strategy to keep the bacteria in check before they can re-establish destructive colonies. Think of it as regular maintenance for a valuable asset—your teeth.
Answering Your Burning Questions (FAQ)
Let's tackle some of the specific, sometimes awkward, questions people are too shy to ask out loud but definitely search online.
Can I smoke after scaling?
This is the tough love section. Smoking is arguably the worst thing you can do for healing gums. It constricts blood vessels, drastically reducing the blood flow and oxygen your gums need to heal and reattach. It also impairs your immune response. The CDC clearly links smoking to gum disease. If there was ever a time to quit or at least pause, it's now. Seriously, it can undermine the entire procedure.
When can I floss again?
You can usually start flossing the untreated areas the next day. For the treated areas, wait until the sharpest tenderness is gone, often around day 3 or 4. When you do, be extra gentle. Use a sawing motion to get the floss between the teeth, then curve it against one tooth and slide it up and down gently, going slightly below the gumline. If it bleeds a little, don't panic—it likely means there's inflammation there that needs cleaning. Consistent, gentle flossing will make the bleeding stop.
My teeth feel loose! Is that normal?
This can be scary. Sometimes, with advanced gum disease, tartar was actually acting like a temporary splint, holding wobbly teeth together. Removing it can make the looseness more apparent initially. As the gums heal, tighten, and reattach, this looseness often improves. However, significant mobility needs to be discussed with your dentist. It's a sign of how much bone support was lost and is a key factor in your long-term prognosis.
How long until I can eat normally?
Use common sense and listen to your mouth. You can gradually reintroduce firmer foods as comfort allows over the first week. By the end of week two, most people are back to their normal diet. Some lingering sensitivity might make you avoid ice cream or hot coffee for a bit longer, but that's about managing comfort, not a healing restriction.
Putting It All Together: Your Mindset Matters
Finally, let's talk psychology. Undergoing periodontal therapy can feel overwhelming. You might feel anxious, or even guilty about the state of your gums. Ditch that guilt. You've taken a massive, positive step by getting treatment. The period of healing—knowing what to expect after periodontal scaling—is your active role in securing a healthier future.
It's not always a linear process. Some days your gums might feel great, others a bit more sensitive. That's okay. The trend over weeks should be positive. Keep your follow-up appointments, be brutally honest with your hygienist about your home care struggles, and celebrate the small wins—less bleeding, less sensitivity, cleaner-feeling teeth.
Arming yourself with knowledge on what to expect after periodontal scaling takes the fear out of the unknown. You've got this. Be patient with your body, meticulous with your care, and stay in close contact with your dental team. Here's to a successful recovery and a much healthier smile.
Leave a Reply