Quick Navigation
- What Exactly Causes Milk Rot Teeth? It's Not Just Milk
- Spotting the Early Signs: Don't Miss the White Spots
- The Professional Fix: What the Dentist Can Actually Do
- The Home Front: Your Daily Role in Fixing and Preventing Milk Rot
- Comparing Your Treatment Options: A Quick Guide
- The Emotional Side: Dealing with Guilt and Moving Forward
- Your Top Questions on Fixing Milk Rot Teeth, Answered
Let's be honest, the first time you hear the term "milk rot teeth" or see a faint white line on your toddler's front teeth, panic sets in. You feel it in your gut. I remember that sinking feeling myself – a mix of guilt and confusion. Was it the bedtime bottle? The sippy cup of milk they carried around all morning? The answer, often, is a complicated yes. But here's the crucial part: that panic doesn't have to turn into despair. Figuring out how to fix milk rot teeth is a journey that starts with understanding, not blame.
Medically, we're talking about Early Childhood Caries (ECC), sometimes called baby bottle tooth decay or nursing caries. It's a specific, aggressive form of decay that can quickly turn from those innocent-looking white spots to brown, broken-down teeth. It hurts. It can affect eating and speaking. And yes, it needs to be addressed.
What Exactly Causes Milk Rot Teeth? It's Not Just Milk
We call it milk rot, but the villain isn't the milk itself. It's the perfect storm of factors. Think of it like this: teeth (even baby ones) are under constant attack. Bacteria in the mouth feed on sugars – from milk, formula, juice, or even sugary snacks. They produce acid. This acid attacks the tooth enamel, the hard outer shell.
Now, with babies and toddlers, the risk skyrockets because of feeding habits. Prolonged exposure is the key. When a child falls asleep with a bottle of milk (or worse, juice), the sugary liquid pools around the front teeth for hours. Saliva flow, which naturally helps wash away sugars and neutralize acid, drops to almost zero during sleep. It's a free pass for acid to do its damage all night long. This is why the classic pattern of "milk rot" shows up on the upper front teeth first – they're bathing in the liquid.
But it's not just bottles. On-demand breastfeeding throughout the night without cleaning the teeth afterward poses a similar risk. So does letting a toddler graze on a sippy cup filled with milk or juice all day long. The teeth never get a break from the acid attacks.
So, the core question for any parent isn't just how to fix milk rot teeth technically, but how to stop the process and create an environment where healing (or at least stabilization) can begin. You have to tackle the cause while you address the damage.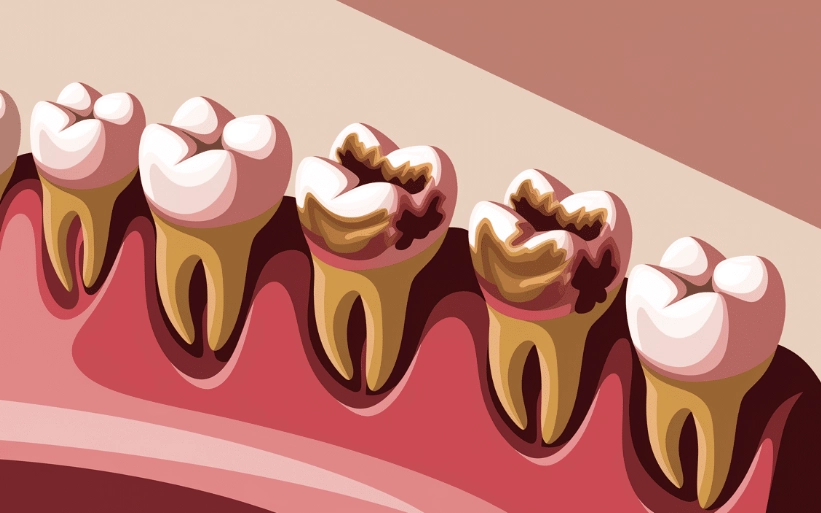
Spotting the Early Signs: Don't Miss the White Spots
Catching this early changes everything. The damage scale is a spectrum, and where your child lands determines the fix.
- The First Alarm (Reversible Stage): Look for dull white bands or spots near the gum line, especially on the upper front teeth. The enamel is losing minerals (demineralizing) but hasn't broken down yet. This stage is crucial! At this point, with major changes in diet and hygiene, you can actually reverse the process and remineralize the enamel. This is the best-case scenario for how to fix milk rot teeth without drills.
- The Progression (Early Cavity): The white spots turn yellowish or light brown. The enamel surface may feel slightly soft or chalky. It's starting to break down.
- The Visible Problem (Cavity): Distinct brown or black holes or pits appear. The tooth structure is compromised. You might notice your child wincing when eating cold, sweet, or hard foods.
- The Advanced Stage: The decay spreads, possibly causing visible broken teeth, swelling in the gums (abscess), or constant pain. This is an urgent dental situation.
If you see anything besides pearly white, don't Google yourself into a frenzy. Just make a dental appointment. A pediatric dentist can use special lights or dyes to see decay much earlier than the naked eye.
The Professional Fix: What the Dentist Can Actually Do
Okay, you've seen the signs and you're at the dentist. What now? The treatment plan depends entirely on the extent of the decay, your child's age, and their ability to cooperate. Let's be real – a two-year-old isn't going to sit still for a complex filling. That's why pediatric dentists have a whole toolkit of approaches.
For Early, Reversible Demineralization (White Spots)
If you're lucky and catch it here, the "fix" is non-invasive and fantastic.
- Fluoride Varnish: This is a sticky, high-concentration fluoride gel painted onto the teeth. It strengthens the enamel and helps it remineralize. It's quick, painless, and done every 3-6 months. The American Dental Association provides extensive resources on fluoride's safety and efficacy in preventing decay (ADA Fluoride Information).
- Silver Diamine Fluoride (SDF): This is a game-changer for halting decay in young kids. It's a liquid brushed onto the cavity. It stops the decay dead in its tracks and hardens the area, but it does turn the decayed spot a dark black or brown (it's permanent on the decay, but doesn't stain healthy enamel). For a small cavity in a fearful toddler, SDF can be a miracle – it avoids drilling and buys time until the child is older. The National Institute of Dental and Craniofacial Research notes its effectiveness as a non-restorative treatment (NIDCR Tooth Decay Info).
For Small to Medium Cavities (The Tooth Structure is Damaged)
Once there's a hole, it needs to be cleaned out and filled.
- Fillings (Restorations): The dentist removes the decayed part and fills it with a tooth-colored composite material. For baby teeth, sometimes stainless steel crowns are used on back teeth if the decay is extensive, as they're more durable.
- The Cooperation Challenge: This is where it gets tricky. A very young, fearful, or uncooperative child may need sedation dentistry. This ranges from nitrous oxide ("laughing gas") to oral conscious sedation, or even general anesthesia in a hospital setting for severe, multiple cavities. It sounds scary, but it allows all the work to be done safely and without creating a lifelong dental phobia.
For Severe Decay (Infections or Unrestorable Teeth)
If the decay has reached the nerve or the tooth is crumbling, options are more limited.
- Pulpotomy ("Baby Root Canal"): If the infection is only in the top part of the nerve, the dentist can remove that infected portion, place a medicated filling, and often cap the tooth with a crown.
- Tooth Extraction: Sometimes, the tooth is too far gone to save. While not ideal, removing a severely infected baby tooth is necessary to stop pain and prevent the infection from harming the permanent tooth below. The dentist will then discuss space maintainers to prevent the other teeth from shifting and crowding the future permanent tooth.
See? The path for how to fix milk rot teeth isn't one-size-fits-all. It's a staircase of interventions.
The Home Front: Your Daily Role in Fixing and Preventing Milk Rot
The dentist provides the repair, but you control the environment. The home care you do is what determines whether the fix lasts or the decay just starts somewhere else. This is the long-term game.
The Feeding Rulebook (The Hardest Part to Change)
- Break the Bottle-to-Bed Habit, Full Stop. This is non-negotiable. If your child needs a bottle to sleep, fill it with water only. The same goes for the naptime bottle. Yes, the first few nights might be rough. It's a short-term struggle for a long-term gain.
- Ditch the All-Day Sippy. Milk and juice are for mealtimes and scheduled snacks, served in an open cup if possible (which minimizes liquid contact with teeth). In between, water is the only drink. This gives teeth a fighting chance to recover from acid attacks.
- Wean Night Feedings. If you're breastfeeding on demand through the night, talk to your pediatrician or dentist about strategies to reduce feeds after the teeth are cleaned for the night.
- Watch the Sticky Snacks. Raisins, fruit snacks, crackers that stick to teeth – they're just as bad as constant milk. Opt for cheese, yogurt, fruits like apples, or veggies.
The Cleaning Protocol (Non-Negotiable Hygiene)
Brushing a toddler's teeth is a battle I know well. But it's a battle you must win.
- Start Early. Wipe gums with a soft cloth before teeth even come in. Use a tiny smear (rice-sized) of fluoride toothpaste as soon as the first tooth erupts. At age 3, you can go to a pea-sized amount.
- You Do the Brushing. Until your child has the manual dexterity to tie their own shoes (around age 6-7), you need to be the one doing a thorough brush, twice a day. They can "practice" after you're done, but the final polish is your job. Get in there and gently brush all surfaces, especially where the gum meets the tooth.
- Floss When Teeth Touch. If two teeth are side-by-side, decay can start between them where the brush can't reach. Use kid-friendly flossers.
- Make it Fun, Not a Fight. Sing songs, use a timer, let them choose a toothbrush with their favorite character. But don't negotiate on whether it happens.
This daily grind of habit change is the real answer to how to fix milk rot teeth for the long haul. The dentist patches the holes, but you build the dam.
Comparing Your Treatment Options: A Quick Guide
When you're sitting in the dentist's chair and they're throwing out terms, it can be overwhelming. This table breaks down the common paths for fixing milk rot teeth.
| Treatment Option | Best For This Stage | What It Does | Pros & Cons (The Real Scoop) |
|---|---|---|---|
| Fluoride Varnish | Very early white spots (demineralization) | Strengthens enamel, can reverse early damage | Pros: Quick, painless, non-invasive, low cost. Cons: Only works if decay hasn't created a cavity yet. |
| Silver Diamine Fluoride (SDF) | Small, early cavities; uncooperative young children | Arrests (stops) active decay, hardens the area | Pros: No drilling needed, great for halting decay fast. Cons: Permanently stains the decayed tissue black. It's a trade-off. |
| Tooth-Colored Filling | Small to medium cavities | Removes decay, restores tooth shape/function | Pros: Natural look, preserves tooth structure. Cons: Requires cooperation/drilling; may not be as durable on baby teeth as crowns. |
| Stainless Steel Crown | Large cavities, especially on back teeth | Caps the entire tooth after decay removal | Pros: Very durable, protects what's left of the tooth. Cons: Silver color is obvious, requires more tooth reduction. |
| Tooth Extraction | Severe, unrestorable decay or infection | Removes the source of pain and infection | Pros: Solves the immediate problem of pain/infection. Cons: Loss of a tooth, may need a space maintainer, can affect chewing. |
Your dentist will recommend a path based on what they see. Don't be afraid to ask why one option is better than another for your specific child.
The Emotional Side: Dealing with Guilt and Moving Forward
Let's talk about the elephant in the room. Parental guilt. It's heavy, and it's almost universal when you're facing a diagnosis of milk rot. You feel like you failed. I felt it. Every other parent I've spoken to in the waiting room has felt it.
But listen – you didn't know. Maybe you were following old advice. Maybe you were just trying to get some sleep. Maybe your child's enamel was just genetically weaker. The cause is almost always a combination of factors.
The most important step you can take now is to learn and act. The fact that you're reading a detailed guide like this means you're already doing that. Beating yourself up doesn't help your child's teeth. Making a plan does. Forgive yourself for the past, and focus your energy on being the advocate and caregiver your child needs for the future. That's the true first step in learning how to fix milk rot teeth – fixing your mindset.
Your Top Questions on Fixing Milk Rot Teeth, Answered
Can milk rot teeth heal on their own?
The very earliest stage – the white spot lesion where minerals have been lost but the surface is intact – can be "healed" or remineralized with fluoride and excellent hygiene. Once the enamel surface breaks and a cavity forms, it cannot heal itself. It's like a small crack in a windshield – it won't fuse back together; it needs a repair.
My child is terrified of the dentist. How can we possibly fix their teeth?
This is the biggest practical hurdle. A good pediatric dentist is part dentist, part psychologist. They use "tell-show-do" techniques, positive reinforcement, and go slow. For necessary work that a child simply can't tolerate while awake, sedation is a safe and compassionate option. It's not a failure; it's a tool to get your child the care they need without trauma.
Are there any natural remedies to fix milk rot teeth?
I'm skeptical of most "natural cure" claims for cavities. Improving diet (less sugar, more whole foods), using xylitol products (which can reduce cavity-causing bacteria), and meticulous cleaning are powerful natural preventative steps. But once a cavity exists, no diet change or oil pulling will make that hole disappear. The decayed tissue needs to be physically removed by a professional to stop the process.
How much will it cost to fix my child's milk rot teeth?
It varies wildly. A fluoride varnish might be under $100. A single filling could be $150-$300. Multiple stainless steel crowns could run over $1,000 per tooth. Treatment under general anesthesia can cost several thousand dollars. Dental insurance helps, but often has limits. Talk to your dentist about a phased treatment plan and payment options. The cost of prevention (toothpaste, brushes, healthy food) is minuscule compared to the cost of repair.
Will fixing the baby teeth affect the permanent teeth?
Yes, but in a good way. Fixing decay and preventing infection protects the permanent teeth developing in the jaw below. A severe infection in a baby tooth can actually damage the enamel of the permanent tooth, causing permanent white or brown spots or deformities. So, fixing the baby teeth is directly protecting the adult smile.
It starts with that first dental visit, continues through the chosen treatments, and lives on in the daily habits you build at home. It's about partnership with your pediatric dentist, consistency in your routine, and letting go of the guilt that holds you back. You now have a map. You know what causes it, how to spot it, what the dentist can do, and what you must do every single day.
The goal isn't perfection – it's progress. It's moving from damage control to lasting health. So take a deep breath, make that appointment, and start. You and your child's smile can absolutely get through this.
Leave a Reply