I've lost count of how many patients have sat in my dental chair, pointed at the white patches on their tongue or the corners of their mouth, and asked with a mix of worry and frustration, "What is this, and how do I make it go away?" That creamy, sometimes painful coating is oral candidiasis, or thrush. And while it's common, the path to getting rid of it isn't always as simple as grabbing a bottle of mouthwash. The biggest mistake I see? People treat the white stuff but ignore what's feeding it.
What You'll Find in This Guide
- What Exactly Is Oral Thrush? (It's More Than Just Yeast)
- Step One: Getting a Proper Diagnosis (Don't Skip This)
- Doctor-Prescribed Oral Candidiasis Treatments Compared
- The Home Care & Prevention Playbook That Actually Works
- When Oral Thrush Signals Something More Serious
- Your Top Thrush Treatment Questions Answered
What Exactly Is Oral Thrush? (It's More Than Just Yeast)
Let's clear something up first. Candida yeast naturally lives in your mouth. The problem isn't its presence; it's an overgrowth. Think of it like weeds in a garden. A few are normal, but when they take over, something's out of balance—too much water, poor soil, not enough sunlight.
For oral thrush, the "garden conditions" that let it run wild are usually:
A disrupted microbiome. This is the big one. Antibiotics are the classic culprit, wiping out the good bacteria that normally keep Candida in check. But it's not just prescription pills. Heavy daily use of alcohol-based mouthwashes can do the same thing—a fact that surprises many of my patients who think they're doing their mouth a favor.
A moist, sugary environment. Candida loves sugar. Poorly cleaned dentures that sit on your gums all night create a perfect, sugary plaque-filled petri dish. Unmanaged diabetes with high blood sugar provides a feast throughout your system.
A weakened local defense. Steroid inhalers for asthma (if you don't rinse after use), smoking, dry mouth from medications, or even just wearing dentures 24/7 which irritates the tissue.
The lesions themselves can vary. The classic is creamy white patches on the tongue, inner cheeks, or roof of the mouth that can be scraped off (sometimes leaving a red, raw area). There's also erythematous (red) candidiasis, which just looks like a sore, red patch, often on the palate under a denture. And angular cheilitis—those painful cracks at the corners of the mouth.
A Non-Consensus Point: Many online guides blame a "weak immune system" as the primary cause. While true for severe cases (like in HIV or cancer treatment), for the average person, it's far more often a local imbalance in the mouth's environment, not a systemic immune failure. Focusing solely on boosting "immunity" misses the practical, immediate fixes like denture hygiene or inhaler technique.
Step One: Getting a Proper Diagnosis (Don't Skip This)
Here's where I see the second biggest error: self-diagnosis. A white tongue can be oral lichen planus, leukoplakia (which can be precancerous), or just debris from poor brushing. Trying oral candidiasis treatments for something that isn't thrush wastes time and money, and delays proper care.
You need a visual diagnosis from a professional—a dentist or a doctor. They can usually tell by looking. In tricky cases, they might gently scrape a sample to look under a microscope or send it for culture. This step is non-negotiable, especially if it's your first time or if the patches don't wipe away easily.
Why is this so critical? Because the treatment your friend used might be wrong for you. The choice of antifungal depends on the severity, location (throat vs. cheeks), and your specific risk factors (like dentures or diabetes).
Doctor-Prescribed Oral Candidiasis Treatments Compared
Once diagnosed, the main arsenal consists of antifungal medications. They work by breaking down the cell walls of the Candida fungus. Don't expect a one-size-fits-all approach. Here’s a breakdown of what your doctor might prescribe, based on what I see work in practice.
| Medication (Type) | How It's Used | Best For / Pros | Cons / Things to Watch |
|---|---|---|---|
| Nystatin Suspension (Liquid) | Swish and swallow (or just swish for infants). 4-5 times daily for 1-2 weeks. | First-line for mild-moderate cases. Tastes okay, local effect. Good for infants. | Frequent dosing is easy to forget. Contains sugar (sucrose), which can be a problem for some. Less effective for severe cases. |
| Clotrimazole Troches (Lozenges) | Let one lozenge dissolve slowly in mouth, 5 times daily for 10-14 days. | Provides prolonged local contact as it dissolves. Sugar-free options available. | Dosing schedule is demanding. Can cause nausea. Not for people who can't safely suck on a lozenge. |
| Fluconazole (Pill) | Oral tablet, typically a single loading dose (200mg) then 100mg daily for 7-14 days. | The heavy hitter. Systemic treatment, reaches all tissues. Simple once-daily dosing. Highly effective for moderate-severe or recurrent thrush. | Potential for more side effects (headache, liver enzyme changes). Drug interactions are common (check with your doctor!). Not the first choice for simple cases. |
| Miconazole Mucoadhesive Buccal Tablet | A tablet placed on the gum above a canine tooth once daily for 1-2 weeks. | Once-daily convenience. Stays in place, slowly releasing medication. | Can cause local irritation or toothache. Not widely available in all countries. |
Treatment length is key. A huge reason for recurrence is stopping medication too early because the white patches are gone. You need to continue for the full prescribed course (often 1-2 weeks) to kill off the remaining yeast. Imagine stopping antibiotics after two days because you feel better—it's the same principle.
Tailored Treatment for Specific Groups
For Denture Wearers: Treating the mouth but not the denture is like treating a fungal foot infection but still wearing the same sweaty socks. Your denture must be disinfected. Soak it overnight in a denture cleaner, but for thrush, you often need a specific antifungal soak. A chlorhexidine solution (like Corsodyl) is effective, but it can stain dentures pink. A diluted bleach soak (1 part household bleach to 10 parts water for 10 minutes) is recommended by the American Dental Association for disinfection, but rinse it extremely well afterward. Discuss the best option with your dentist.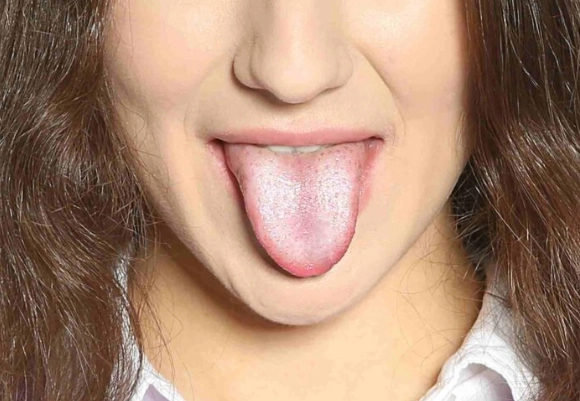
For Babies & Breastfeeding Mothers: It's a ping-pong game. The baby gets treated with nystatin drops applied inside the mouth. But if the mother is breastfeeding, she likely has a candidiasis infection on her nipples (often burning, shiny red skin), which will reinfect the baby. She needs a topical antifungal cream (like miconazole) on her nipples. Treat both simultaneously.
For People Using Steroid Inhalers: Always, always rinse your mouth with water (and spit) after each use. Consider using a spacer device with your inhaler, which reduces the amount of medication that coats your mouth and throat.
The Home Care & Prevention Playbook That Actually Works
Medication knocks the infection down, but your daily habits determine if it comes back. This is the 80/20 rule of oral candidiasis treatments—the meds are 20%, the aftercare is 80%.
Your Daily Thrush-Prevention Checklist
- Oral Hygiene Reset: Replace your toothbrush, tongue scraper, and denture brush after you finish your medication. You don't want to re-inoculate yourself.
- Denture Overnight Protocol: Dentures out at night. Soak in an effective cleanser. This gives your gum tissue a chance to breathe and recover.
- Dietary Tweaks (Temporarily): Reduce refined sugars and yeasty foods (bread, beer, wine) while treating an active infection. It starves the yeast. Probiotic yogurt with live cultures can help repopulate good bacteria.
- Gentle, Non-Disruptive Rinses: Instead of harsh alcohol mouthwashes, use a warm saltwater rinse (1/2 tsp salt in a cup of water) or a baking soda rinse (1/2 tsp baking soda in a cup of water). These soothe tissue and make the oral environment less acidic, which Candida dislikes.
- Manage Dry Mouth: If medications cause dry mouth, sip water, use sugar-free lozenges, or ask your doctor/dentist about saliva substitutes. A dry mouth is a vulnerable mouth.
When Oral Thrush Signals Something More Serious
Most oral thrush is a localized nuisance. But sometimes, it's a red flag. You should seek prompt medical attention if:
The infection is severe, making it painful to swallow or eat. This can lead to dehydration and malnutrition.
It spreads down your throat (esophageal candidiasis). This feels like food is getting stuck or pain behind the breastbone.
You have recurrent episodes (more than 2-3 times a year) without an obvious cause like antibiotic use. This warrants investigation into potential underlying conditions like undiagnosed diabetes, nutritional deficiencies (iron, B12, folate), or, rarely, immune disorders. A study published in the journal Clinical Infectious Diseases notes recurrent oral candidiasis can be an early sign of immune dysfunction.
The patches are irregular, hardened, or don't scrape off. This needs a biopsy to rule out other conditions.
Your Top Thrush Treatment Questions Answered
What is the fastest way to get rid of oral thrush?
The fastest resolution typically comes from prescription antifungal medications like fluconazole (a single-dose pill) or clotrimazole troches. However, speed depends on the underlying cause. If you're on a steroid inhaler and don't rinse properly, even strong medication will be less effective. Addressing the root trigger is part of the speed equation.
Can I treat oral candidiasis at home without seeing a doctor?
For a very mild, first-time case, gentle saltwater rinses and meticulous oral/denture hygiene might help. But oral thrush often signals an imbalance. Self-treating risks missing underlying issues like diabetes or immune changes. If symptoms persist beyond 3-4 days, or if you have difficulty swallowing, see a doctor or dentist. Over-the-counter options are limited and often ineffective for established infections.
My oral thrush keeps coming back after treatment. What am I doing wrong?
Recurrence is frustrating and points to a persistent reservoir or trigger. Common overlooked culprits include: 1) Dentures not being soaked overnight in an antifungal cleaner, 2) Not replacing your toothbrush or tongue scraper after treatment, 3) Unmanaged acid reflux introducing stomach yeast, or 4) An underlying health condition that hasn't been stabilized. A longer, low-dose maintenance course of medication is sometimes needed.
Are natural remedies like coconut oil or apple cider vinegar effective for oral thrush?
The evidence is anecdotal. Coconut oil has antifungal properties in lab studies, but its clinical effect in the mouth is unproven. Swishing with apple cider vinegar is risky—its acidity can damage tooth enamel and irritate already-sensitive tissues, potentially worsening the condition. These should not replace medical treatment. Gentler, evidence-supported supportive measures include probiotic yogurt (with live cultures) and baking soda rinses to alter the oral pH.
Successfully treating oral candidiasis is a two-part process: attack the overgrowth with the right medication, and then change the environment that allowed it to flourish. It's not just about what you put in your mouth for a week, but what you do every day afterward. If you tackle both, that uncomfortable white coating can become a thing of the past.
Leave a Reply