You know that feeling. You wake up and your jaw feels tight, like you've been chewing gum all night. Or maybe there's a dull ache in your temples that coffee just won't shake. For some, it's a mysterious chip in a tooth with no memory of an accident. If this sounds familiar, you're likely dealing with bruxism—the medical term for grinding or clenching your teeth. But here's the tricky part: the most damaging bruxism symptoms are often the ones you'd never think to connect to your teeth.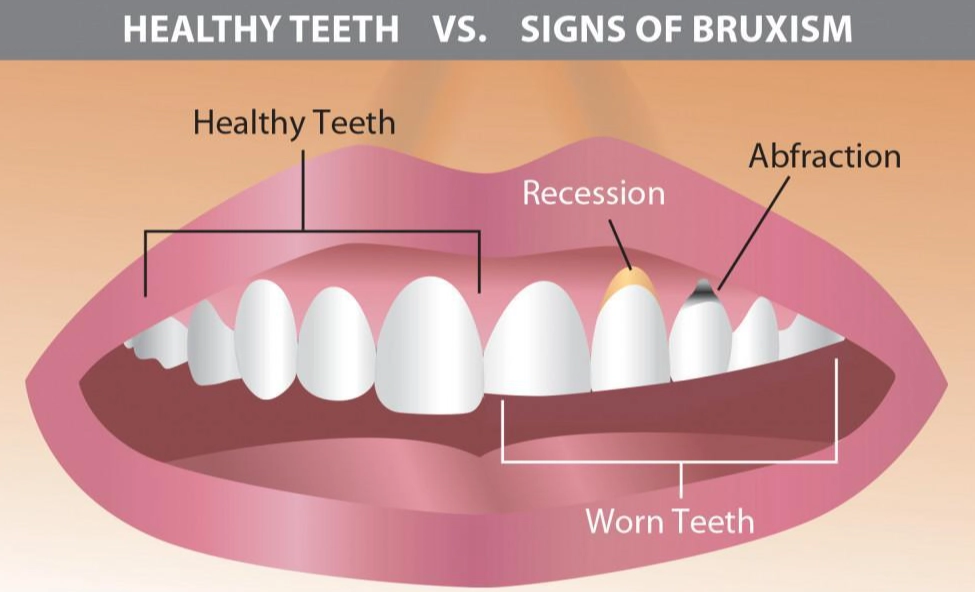
I've worked with patients who came in for chronic headaches, only to find the root cause was their jaw. Others were convinced they had an ear infection. The symptoms masquerade as other problems, which is why so many people suffer for years without a clear answer.
What You’ll Discover in This Guide
What Are the Most Common Bruxism Symptoms?
Let's break this down into what you can feel and what you (or your dentist) can see. Most people only recognize a fraction of the signs.
The Obvious Signs (The Ones You Feel)
These are the symptoms that will have you searching for answers online.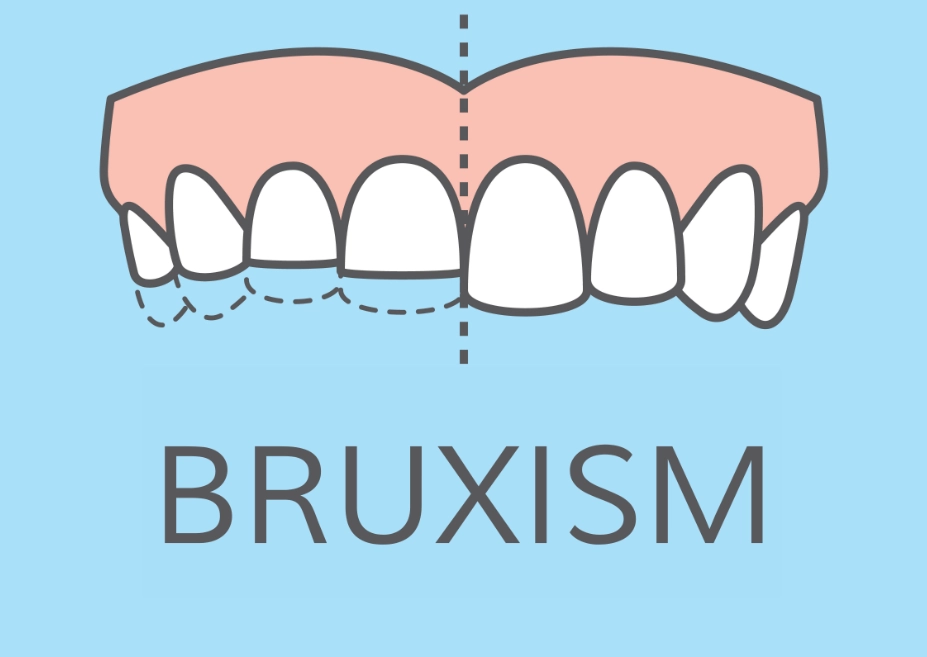
- Jaw, face, or ear pain: This isn't always sharp. It's often a soreness, a stiffness in the muscles along your jawline (the masseters), or a deep ache that seems to come from your ear. It’s usually worst in the morning.
- Morning headaches: Specifically, tension-type headaches that start at your temples or the back of your head. The American Academy of Sleep Medicine lists this as a key indicator of sleep bruxism.
- Locked or clicking jaw: If your jaw pops when you open wide or, worse, feels like it gets stuck, your temporomandibular joints (TMJs) are under stress from clenching.
- Tooth sensitivity: A sudden wince with hot coffee or ice cream. This happens because grinding wears down the protective enamel, exposing the sensitive dentin underneath.
The Silent Signals (The Ones You See or Hear)
These are the clues you need to look for, or that someone else might notice.
- Flattened, chipped, or fractured teeth: Check your back molars. Are the pointed cusps worn down flat? Do the edges of your front teeth look uneven or see-through? This is slow-motion destruction.
- Increased tooth mobility: Your teeth shouldn't feel loose. Chronic, extreme force can stretch the periodontal ligament that holds them in place.
- Worn dental work: Crowns, fillings, or implants that show unusual wear or cracks are a major red flag.
- Audible grinding sounds: This is the classic sign a sleep partner reports. It can sound like scraping, crunching, or tapping. If you live alone, audio recording your sleep (with various apps) can reveal it.
- Cheek biting or scalloped tongue: Look at the inside of your cheeks for ragged white lines. Your tongue's edges might show indentations from being pressed constantly against your teeth.

A Quick Self-Check: Run your tongue over the biting surfaces of your back teeth. Do they feel sharp and defined, or smooth and rounded? Smoothness is often the first sign of wear, long before pain or sensitivity starts.
How Bruxism Symptoms Impact Your Overall Health
This is where most articles stop. They list the symptoms but don't connect the dots to your wider well-being. Bruxism isn't just a dental issue; it's a full-body stress response.
Think of your jaw as the crossroads of several major systems. The trigeminal nerve, one of the largest cranial nerves, runs through it. When you clench, you're not just tightening one muscle. You're activating a chain that leads to tension headaches, can contribute to tinnitus (ringing in the ears), and even affect your posture. You might start subconsciously tilting your head forward to compensate for jaw tension, leading to neck and shoulder pain.
The sleep disruption is another hidden cost. Even if the grinding doesn't fully wake you, it can pull you out of deep, restorative sleep stages. You might sleep for 8 hours but wake up feeling unrefreshed. The research isn't entirely settled, but studies, including some referenced by the National Institutes of Health, suggest a complex bidirectional relationship between sleep bruxism and other sleep disorders like sleep apnea.
Then there's the psychological toll. Chronic pain from your jaw or head can increase stress and anxiety, which in turn can make you clench more. It's a vicious cycle.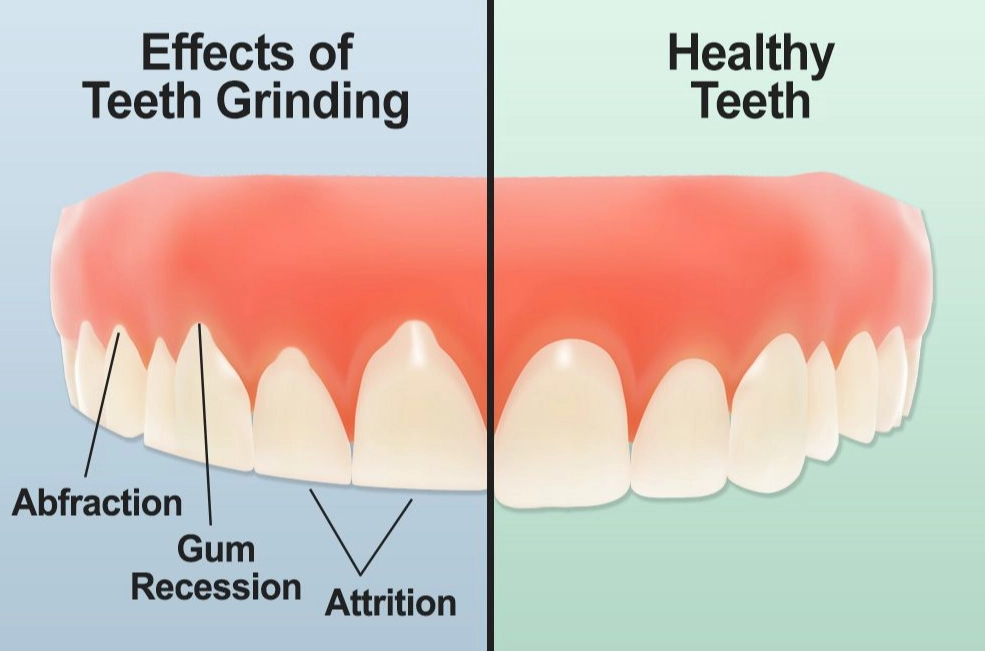
How to Get a Proper Diagnosis for Bruxism
So you have some symptoms. What now? A proper diagnosis is a two-part process: a clinical exam and identifying the likely triggers. Many dentists will jump straight to a night guard, but a good one will play detective first.
The Dental Exam: Your dentist should do more than just a quick look. They'll feel your jaw muscles for tenderness, listen and feel for clicks or pops as you open and close, and use a small ruler to measure your range of motion. They'll examine your teeth under bright light, possibly with magnification, for wear patterns that are the fingerprint of bruxism. They might take impressions or digital scans to monitor wear over time.
The Trigger Assessment: This is the conversation. Be prepared to talk about:
- Stress levels: Work, family, life events.
- Sleep habits and quality: Do you snore? Feel tired all day?
- Medications: Certain SSRIs (a common class of antidepressants) are known to increase bruxism.
- Lifestyle factors: Alcohol, recreational drugs, and even excessive caffeine can aggravate it.
- Anatomy: Misaligned teeth or an irregular bite can be contributing factors.
For severe or complex cases, a dentist might refer you to a specialist like an orofacial pain doctor or a sleep physician. A sleep study (polysomnography) is the gold standard for diagnosing sleep bruxism, as it can measure the actual muscle activity in your jaw during sleep, but it's not always necessary for a basic diagnosis and initial treatment.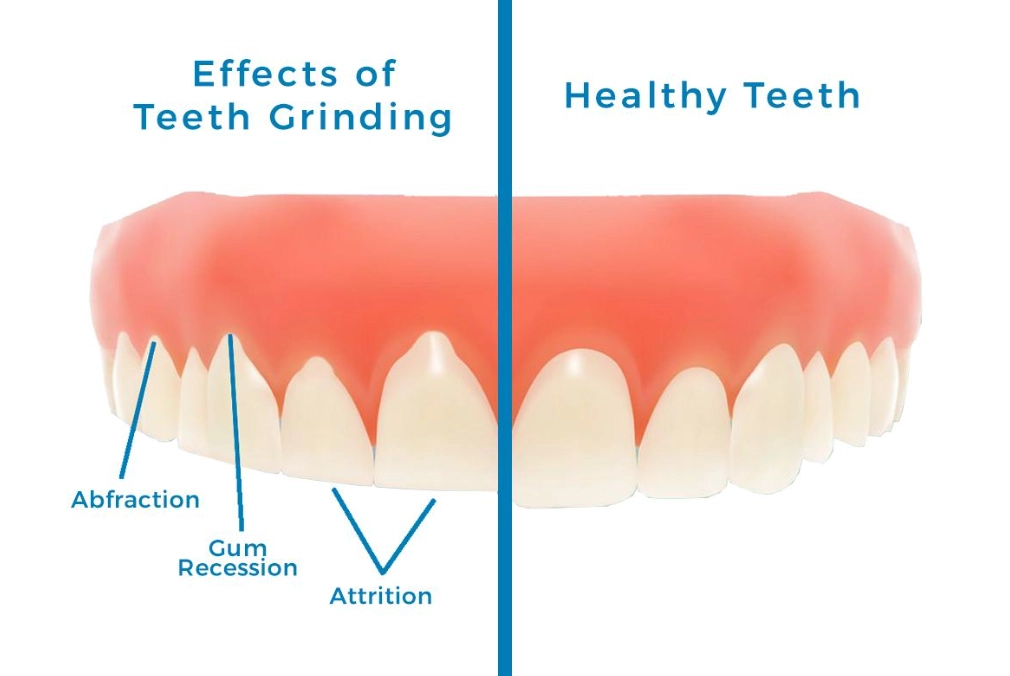
One common mistake I see: People buy cheap, boil-and-bite night guards from the pharmacy. These can often make things worse. They're bulky, can encourage more chewing motion, and if not fitted properly, can actually push your teeth out of alignment. A custom-made guard from your dentist is thinner, more comfortable, and designed to protect your teeth without altering your bite.
Treatment Options: Moving Beyond the Basic Night Guard
Treatment isn't one-size-fits-all. It's a layered approach, starting with protection and moving toward addressing the root cause. Here’s a practical breakdown of the options, from immediate relief to long-term management.
| Treatment Approach | What It Involves | Best For... | Considerations |
|---|---|---|---|
| Protection (The Guard) | Custom-fitted oral appliance worn at night. Made of hard acrylic, it creates a barrier between upper and lower teeth. | Everyone with confirmed tooth wear or damage. It's the first line of defense to stop the destruction. | Not a cure. Prevents damage but doesn't stop the clenching impulse. Requires cleaning and occasional replacement. |
| Behavioral & Lifestyle | Stress management (meditation, therapy), jaw exercises, reducing stimulants (caffeine, nicotine), improving sleep hygiene. | Awake bruxism and mild sleep bruxism. Essential for addressing underlying triggers. | Requires consistent effort and self-awareness. The "jaw posture" trick (lips together, teeth apart, tongue on roof of mouth) is a simple daily habit. |
| Physical Therapy | Targeted massage, stretching, ultrasound, or dry needling on jaw and neck muscles by a PT specializing in TMJ. | Significant muscle pain, limited jaw movement, or associated neck/shoulder tension. | Can provide dramatic pain relief. Often used in combination with other therapies. |
| Medical Interventions | Muscle relaxants (short-term), Botox injections into the masseter muscles, adjusting medications that may cause bruxism. | Severe, drug-resistant cases where muscle hypertrophy (enlargement) is evident. Botox weakens the clenching force. | Botox is temporary (lasts 3-4 months), can be costly, and should be administered by an experienced professional. |
| Addressing Sleep Issues | Evaluation for sleep apnea. Treatment with a CPAP machine if apnea is diagnosed. | Patients with loud snoring, witnessed breathing pauses, and severe morning symptoms. | Treating sleep apnea can significantly reduce or eliminate sleep bruxism in many cases. |
The journey usually starts with the guard and lifestyle changes. Give it 3-6 months. If symptoms persist, that's when you layer on the next approach, like PT or a sleep study. It's about building your personal toolkit.
I had a patient, let's call her Sarah, a graphic designer with awful morning headaches. She got a guard but saw little improvement. We dug deeper and realized her clenching peaked during intense, deadline-driven work at her computer. We added in a posture check (she was hunching), scheduled 5-minute "jaw check" breaks every hour where she'd do a few stretches, and she started using a stress ball. The combination of the guard (for night) and the daytime habits finally broke the cycle for her.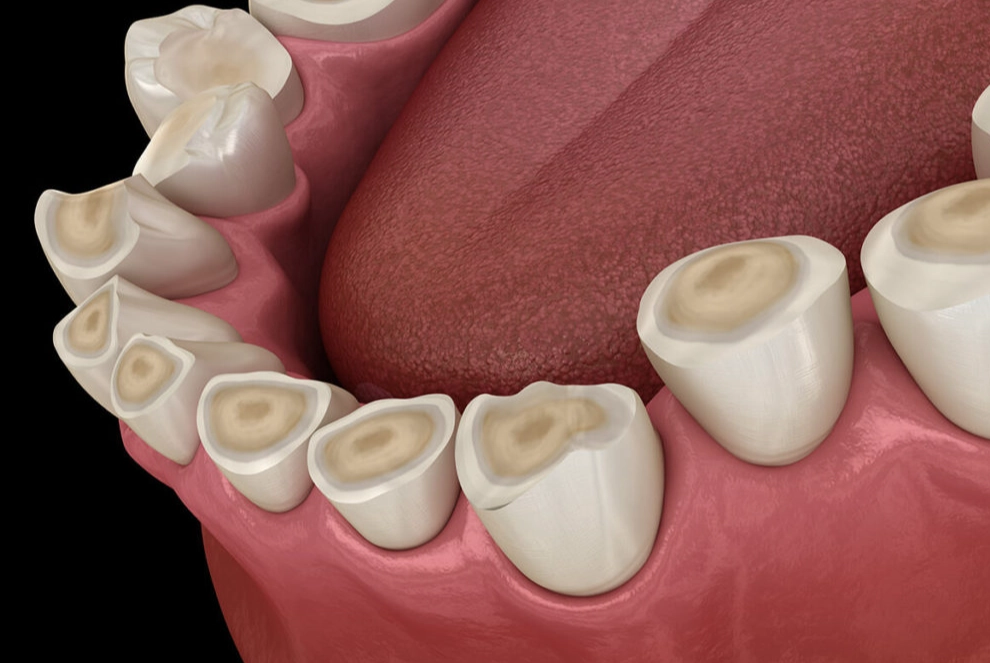
That's the key. It's rarely just one thing.
 Recognizing bruxism symptoms is the first, crucial step out of a cycle of pain and damage. It's a common issue, but its presentation is uniquely personal. Stop dismissing that jaw tightness or morning headache as normal. Pay attention to the signals your body is sending, get a professional evaluation, and start building your multi-layered plan for relief. Your teeth—and the rest of you—will thank you for it.
Recognizing bruxism symptoms is the first, crucial step out of a cycle of pain and damage. It's a common issue, but its presentation is uniquely personal. Stop dismissing that jaw tightness or morning headache as normal. Pay attention to the signals your body is sending, get a professional evaluation, and start building your multi-layered plan for relief. Your teeth—and the rest of you—will thank you for it.