Quick Guide to Gum Health
You're brushing your teeth, minding your own business, when you see it. A tiny red dot on the gum above your tooth. It wasn't there yesterday. Or maybe it was, and you're just noticing it now. Your mind starts racing. Is it serious? Is it an infection? Should you call the dentist right now, or can you just rinse with salt water and hope it goes away?
Let's take a breath. I've been there myself. A few years back, I spotted one of these little red dots near a molar and completely overreacted, convinced it was a sign of something catastrophic. Turns out, it was just a minor irritation from a popcorn hull. But it taught me a valuable lesson: not every tiny red dot on gum above tooth is a disaster, but ignoring them isn't smart either.
The truth is, that small spot is your body sending a signal. Sometimes it's a whisper, sometimes it's a shout. Your job is to figure out which one it is. This guide is here to help you do exactly that. We'll walk through everything—from the totally harmless causes to the ones that need a dentist's attention, pronto. We'll talk about what you can do at home, what a dentist will do, and how to stop these dots from showing up in the first place.
What Exactly Is This Tiny Red Dot? Breaking Down the Possibilities
First things first, let's demystify it. A tiny red dot on gum above tooth is essentially a localized area of inflammation or irritation. The redness comes from increased blood flow to the area—your immune system sending troops to check out a potential problem. But what's triggering the response? The list is longer than you might think.
It's not always a single thing. Often, it's a combination. Maybe you brushed too hard and have a bit of plaque buildup. The table below breaks down the common culprits, from most frequent to less common, so you can start to match your symptoms.
| Possible Cause | What It Typically Looks/Feels Like | Common Triggers | Urgency Level |
|---|---|---|---|
| Localized Gingivitis | A small, red, sometimes slightly puffy dot. Gums may bleed a little when flossing that specific spot. No pain usually. | Plaque buildup in one area, missed by brushing/flossing. | Low (but needs addressing) |
| Minor Physical Irritation or Trauma | A pinpoint red or dark red dot. Might feel tender if touched. Could have a tiny scratch nearby. | Poking with a toothpick, sharp food (chip, popcorn hull), aggressive brushing, ill-fitting dental appliance. | Low |
| Beginning of a Gum Abscess (Periodontal Abscess) | A red dot that may have a yellowish or white center (pus). The gum around it is swollen, tender to touch, and often throbs with pain. You might feel a bad taste. | Deep infection in the gum pocket next to the tooth, often in someone with existing gum disease. | High - See a dentist |
| Canker Sore (Aphthous Ulcer) on the Gum | Starts as a red spot, quickly develops a white or yellow center with a red halo. Can be quite painful, especially with acidic foods. | Stress, minor injury, acidic foods, vitamin deficiencies. | Low-Medium (pain management) |
| Hormonal Fluctuation Spot | Generalized or localized redness and swelling, may appear as isolated dots. Gums feel spongy and bleed easily. | Puberty, menstruation, pregnancy, certain birth control pills. | Low (monitor) |
| Allergic Reaction | Red dot or patch, possibly itchy. Surrounding gum might also be red. | New toothpaste (e.g., whitening agents like pyrophosphates), mouthwash, dental materials, certain foods. | Medium (identify & remove trigger) |
See? It's a mixed bag. The tiny red dot on gum above your tooth from flossing too hard looks different and means something totally different than one caused by a brewing infection.
I remember a friend who swore her red dot was a cancer scare. The anxiety was awful. After a dental visit, it turned out to be a simple reaction to a new, overly-strong mouthwash she'd bought. She switched back to her old one, and the dot faded in a few days. The lesson? Don't jump to the worst conclusion first.
When Should You Actually Worry? Red Flags You Can't Ignore
Okay, so most of the time it's not an emergency. But how do you know when it is? This is the part where you need to be your own best observer. Some signs are your mouth's way of waving a red flag.
Let's be clear: pain is a big indicator. A tiny red dot on gum above tooth that's just sitting there quietly is less concerning than one that throbs, aches, or sends a sharp pain when you bite down. Pain means inflammation or infection is putting pressure on nerves.
- Persistent, Throbbing Pain: This is the hallmark of an abscess. The pressure from pus buildup hurts, often a lot.
- Visible Swelling: Not just the dot, but the gum around it is puffed up like a pillow. Swelling in your face or jaw is a major emergency.
- Pus or Discharge: If you see white/yellow material or feel a foul taste/smell, that's infection.
- Fever: Your body is fighting a systemic infection. Don't wait.
- The Dot is Growing or Changing Fast: What was pin-sized yesterday is pea-sized today.
- A Loose Tooth: If the tooth near the dot feels wiggly, the supporting bone may be affected.
No joke, an untreated dental abscess can spread. It's rare, but it can lead to serious infections in other parts of your body. The Mayo Clinic outlines the potential complications, which is why they stress not ignoring significant symptoms.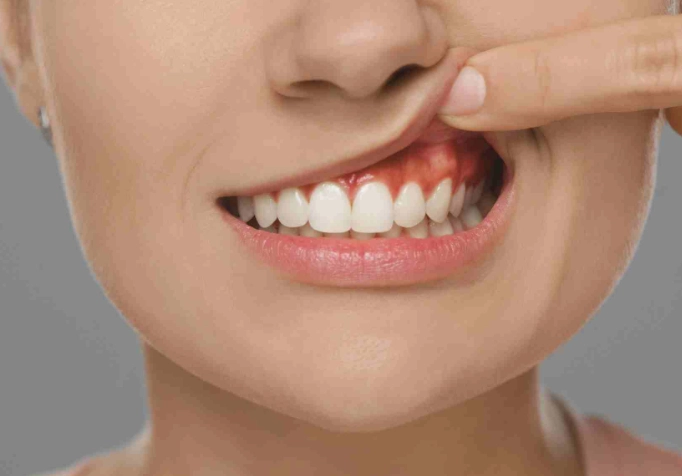
On the flip side, if the dot is painless, hasn't changed in a week, and your gums otherwise look pink and firm, you likely have time to monitor and improve your home care. But monitor actively—don't just forget about it.
What a Dentist Will Do: The Diagnosis Process Demystified
If you decide to see a dentist (which is the smart move for any persistent or painful dot), here's what to expect. It's not scary, just thorough. They're playing detective.
First, they'll ask you questions. When did you first see it? Does it hurt? Have you changed any products? They'll then do a visual exam with those little mirrors and lights. They're looking at the color, size, and shape of the dot and the surrounding tissue.
The next tool is often a periodontal probe. This is a tiny ruler they gently place between your tooth and gum. They're measuring the pocket depth. Healthy pockets are 1-3 millimeters deep. Deeper pockets (4mm+) can trap debris and bacteria, leading to the kind of infection that causes a red, swollen dot. If they call out numbers like "five" or "six" near that tooth, that's a key clue.
They might press gently around the area to see if pus emerges—a sign of an abscess. Sometimes they'll take a dental X-ray, usually a periapical film that focuses on that one tooth and its root and bone. This is crucial. It can reveal an abscess at the root tip (a different type) or show if the bone supporting the tooth has been damaged by gum disease, which the American Academy of Periodontology notes is a leading cause of tooth loss in adults.
Based on this detective work, they'll give you a diagnosis. It might be "localized gingivitis," "periodontal abscess," or "traumatic lesion." The name dictates the treatment.
Treatment Paths: From Home Care to Professional Procedures
So what happens after the diagnosis? The treatment plan depends entirely on what's causing your specific tiny red dot on the gum above your tooth.
For Minor Irritation or Gingivitis:
The dentist or hygienist will likely do a professional cleaning, focusing on that area to remove the plaque and tartar (calculus) that's irritating the gum. They'll then give you targeted home care instructions. This isn't just "brush better." It might be:
- Using a soft-bristled toothbrush and angling it 45 degrees toward the gumline.
- Demonstrating how to floss correctly—curing the floss around the tooth and going slightly below the gumline, not just snapping it up and down.
- Suggesting an antimicrobial mouthwash like one containing chlorhexidine (by prescription) or essential oils like cetylpyridinium chloride (over-the-counter) for a short period to reduce bacteria.
- Recommending a water flosser to gently flush out the area if traditional flossing is difficult.
For a Gum Abscess:
This requires professional intervention. The goal is to drain the infection and clean out the source. The dentist will likely:
- Drain the abscess: They may make a small incision in the gum to let the pus drain out, which provides immediate pain relief.
- Scale and root planing: This is a deep cleaning under local anesthesia. They clean the infected pocket thoroughly, removing tartar and bacteria from the tooth root surface. This is the cornerstone of non-surgical periodontal therapy.
- Antibiotics: These aren't always needed if the infection can be fully drained and cleaned. But for severe or spreading infections, they may prescribe them. It's worth noting the CDC promotes antibiotic stewardship in dentistry, meaning they are used judiciously, not as a first-line cure for every issue.
In more advanced cases of gum disease where deep pockets persist, other procedures like gum surgery or laser therapy might be discussed. But for that initial tiny red dot on gum above tooth, it rarely gets to that stage if caught early.
Stopping the Dots Before They Start: Prevention is Everything
This is the most important chapter. The best way to deal with a problem is to prevent it from happening. Most causes of these red dots are preventable with consistent, good oral hygiene. Not perfect, just good and consistent.
It starts with the basics, but doing them right. Brushing twice a day for two minutes with a fluoride toothpaste and a soft brush. Flossing once a day—and I mean every day, not just when you feel something stuck. The plaque that causes gingivitis and worse hardens into tartar in about 24-48 hours. Tartar is cement-like; you can't brush or floss it off. Only a dental professional can remove it.
Your diet plays a sneaky big role. Sugary and starchy foods feed the bacteria in plaque. These bacteria produce acids and toxins that inflame your gums. It's not about never having sugar, but about not letting it sit on your teeth for long periods. Drinking water, especially after meals, helps rinse things away.
Don't smoke or use tobacco products. This is a huge one. Smoking wreaks havoc on your gums. It reduces blood flow, masking the redness and bleeding of gingivitis (so problems are hidden longer), and severely compromises your immune system's ability to fight gum infections. It's a double whammy.
And finally, see your dentist for regular check-ups and cleanings. For most people, that's every six months. If you have a history of gum issues, they might recommend every 3-4 months. These visits aren't just for cleaning; they're for catching a tiny red dot on gum above tooth when it's just a whisper, long before it becomes a shout.
I made the switch to an electric toothbrush a few years ago, and my hygienist noticed a difference at my next cleaning. My gums were less inflamed. It's not magic, but the consistent motion and timer helped me clean more effectively without brushing too hard.
Your Questions, Answered: The Tiny Red Dot FAQ
Look, finding something unexpected in your mouth is unsettling. But knowledge is power. That tiny red dot on gum above your tooth is information. Use this guide to understand what it might be telling you, take the appropriate action, and then get back to your life with a healthier, happier mouth. Pay attention, but don't panic. And when in doubt, let a professional take a look. It's what they're there for.