Your Quick Guide
- What Exactly Is Happening in There? The Anatomy of an Infected Tooth
- How Do You Know It's Infected? The Symptom Checklist
- What Causes Teeth to Get Infected in the First Place?
- What Can You Do at Home? (The Realistic Guide)
- What Will the Dentist Do? The Professional Treatment Playbook
- What Happens If You Just Ignore It? The Domino Effect of Complications
- How to Prevent Infected Teeth in the First Place
- Common Questions About Infected Teeth (Answered)
Let's be honest, nothing throws your life off track quite like a toothache that turns into something worse. One minute you're enjoying a meal, the next you're wincing with a pain that feels like a tiny, angry drum solo happening inside your jaw. I've been there. That dull ache that you keep hoping will just go away on its own, only to wake up one night with your face feeling swollen and tender. It's a special kind of misery.
That misery usually has a name: an infected tooth. Or maybe your dentist calls it an abscessed tooth, a dental abscess, or a periapical infection. They all point to the same scary reality – bacteria have invaded the inner sanctum of your tooth, the pulp, and set up camp. Your body's fighting back, and the battleground is your mouth. Not a fun place to be.
This guide isn't here to scare you. It's here to cut through the confusion. We'll walk through exactly what's happening, how to spot the signs before it gets bad, what you can actually do about it right now, and what the dentist will likely recommend. Think of it as your roadmap from "Uh oh" to "Okay, handled."
What Exactly Is Happening in There? The Anatomy of an Infected Tooth
To understand the infection, you need to know the layers of a tooth. On the outside, you have the hard enamel – the toughest stuff in your body. Under that is dentin, which is softer and has tiny tubes leading inward. At the core is the pulp. This is the tooth's living room. It's packed with nerves, blood vessels, and connective tissue. It's how the tooth senses hot and cold, and it keeps it nourished.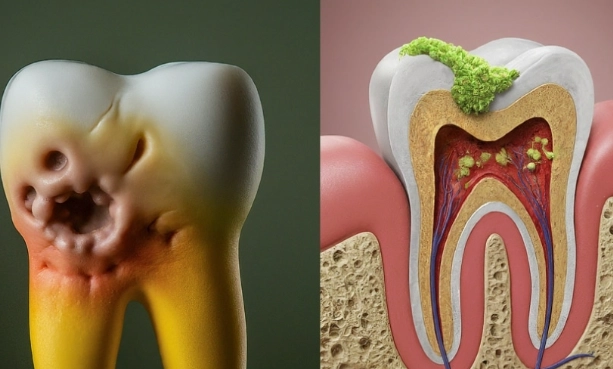
An infected tooth starts when bacteria breach the defenses. This usually happens through:
- A deep cavity that's been ignored for too long (the most common culprit).
- A crack or chip in the tooth from an injury or just wear and tear.
- Advanced gum disease (periodontitis), where the infection comes up from the gums rather than down from the crown.
Once the bacteria get into the pulp, it's game on. The pulp gets inflamed (that's pulpitis, which can be reversible or, more often, irreversible). Then it starts to die. As the pulp tissue breaks down, the bacteria multiply and push their way out through the very tip of the tooth root. This forms a pocket of pus – the abscess. That pus has nowhere to go, so it creates pressure. And that pressure? That's the source of most of your intense, throbbing pain. The pressure stimulates the nerve endings in the ligament holding your tooth in place and can even start eating away at the jawbone itself.
How Do You Know It's Infected? The Symptom Checklist
Not every toothache means a full-blown infection. Sometimes it's just sensitivity. But there are red flags. Here’s what to watch for, moving from early warnings to full-blown emergency signs.
The Early Warnings (Don't Ignore These!)
- Persistent Toothache: Not just a twinge when you sip ice water, but a constant, dull, or throbbing ache that doesn't quit. It might even wake you up at night.
- Temperature Sensitivity: Pain that lingers for more than a few seconds after having something hot or cold. A hot drink making it worse can be a particularly telling sign of a dying nerve.
- Pain When Chewing or Pressing: If biting down sends a sharp jolt, it's a sign the infection is affecting the structures around the root.
- A Small Bump on the Gums: You might feel a pimple-like bump near the sore tooth. This is called a fistula or a gum boil, and it's actually a drainage channel for the pus. Sometimes it bursts, you get a bad taste, and the pain lessens temporarily – but the infection is still very much there.
The "Get to a Dentist NOW" Signs
- Swelling in Your Face, Cheek, or Jaw: This means the infection is spreading. It can look like you have a chipmunk cheek.
- Swollen Lymph Nodes: Under your jaw or in your neck feeling tender and swollen.
- Fever: Your body is mounting a full-scale immune response to the infection.
- Difficulty Swallowing or Breathing: This is rare but serious. Swelling in the floor of the mouth or neck (Ludwig's Angina) can become life-threatening by blocking airways.
I remember once putting off a dentist visit with a sore tooth because I was "too busy." The swelling came on fast. My cheek puffed up, and I felt generally awful. The dentist later told me the infection was close to spreading into deeper facial spaces. It was a stupid gamble I won't take again. The pain and cost of treating a full-blown infected tooth are far worse than dealing with a cavity early.
What Causes Teeth to Get Infected in the First Place?
Understanding the causes is the first step to prevention. It's not just about candy (though that doesn't help).
- Untreated Cavities: The champion cause. Plaque acids create holes, bacteria march in. Simple as that.
- Dental Trauma: A knocked-out or cracked tooth can expose the pulp immediately or slowly over time as the crack deepens.
- Failed Dental Work: Sometimes, an old filling or crown can fail, allowing leakage and bacteria to sneak in. It's frustrating, but it happens.
- Severe Gum Disease:
This is a different path. Here, the infection starts in the gum pocket next to the tooth and works its way down to infect the root from the side. This is called a periodontal abscess.
What Can You Do at Home? (The Realistic Guide)
Okay, it's 10 PM, your tooth is killing you, and the dentist opens at 8 AM. What now? Let's separate helpful home care from harmful myths.
What Actually Helps Manage the Pain
- Over-the-Counter Pain Relievers: Ibuprofen (Advil, Motrin) is often better than acetaminophen (Tylenol) for dental pain because it reduces inflammation. Important: Always follow label directions and never place the pill directly on the gum—it can burn the tissue.
- Cold Compress: Apply an ice pack wrapped in a cloth to the outside of your cheek for 15-minute intervals. This helps reduce swelling and numbs the area.
- Salt Water Rinse: Dissolve half a teaspoon of salt in a glass of warm water. Swish gently for 30 seconds. This can help draw out some fluid, soothe inflamed gums, and is mildly antiseptic. Do this a few times a day.
- Elevate Your Head: When you sleep, prop yourself up with an extra pillow. Lying flat can increase blood pressure to the area, making the throbbing worse.
What to Avoid (Seriously, Don't Do This)
- Putting Aspirin on the Tooth: An old wives' tale that causes chemical burns on your gums. Swallow it if you need to, don't topicalize it.
- Using Heat: A warm compress might feel good momentarily, but heat increases blood flow and can worsen swelling and spread the infection.
- Poking the Area: Don't try to pop a gum boil yourself. You'll likely push bacteria deeper.
- Sugary or Extremely Hot/Cold Foods & Drinks: They will aggravate the pain.
What Will the Dentist Do? The Professional Treatment Playbook
This is the part people dread, but knowing what to expect takes away a lot of the fear. The goal of treatment is to eliminate the infection and save the tooth if possible. The path depends on how bad the damage is.
First Line of Defense: Antibiotics
If there's significant swelling or fever, the dentist will likely prescribe antibiotics like amoxicillin or clindamycin (if you're allergic to penicillin). This is crucial to control the systemic infection and reduce swelling before they can do the definitive treatment. But here's the critical point everyone misses:
The Definitive Treatments: Saving or Removing the Tooth
Once the infection is under control, you have two main options. Let's break them down in a table because it's easier to compare.
| Treatment | What It Is | Pros | Cons / Considerations | Best For... |
|---|---|---|---|---|
| Root Canal Treatment (RCT) | The dentist makes a small opening, removes all the infected pulp, cleans and disinfects the inside canals, then fills and seals them. A crown is usually placed later to protect the now-brittle tooth. | Saves your natural tooth. Preserves jawbone and bite. Looks and functions like a normal tooth. | Can be costly. Requires multiple visits. The tooth is no longer "alive" and can become brittle. | Teeth where the structure is still largely intact. The preferred method to save a tooth with an infected pulp. |
| Tooth Extraction | The entire tooth is removed. The socket heals over time. | Permanently removes the source of infection. Usually less expensive upfront than RCT + crown. | You lose the tooth. Can lead to bone loss, shifting of other teeth, and bite problems. Requires replacement (implant, bridge, denture) to avoid issues. | Teeth that are too broken down to save, or if the patient cannot afford/undergo a root canal. |
Most dentists, including the American Dental Association (ADA), will recommend a root canal to save a salvageable tooth. It has a very high success rate. Extraction should be a last resort. I had a root canal years ago on a molar. Was I excited? No. But it was either that or lose the tooth. Ten years later, that tooth is still doing its job perfectly, with no pain. The procedure itself was no worse than a large filling.
What Happens If You Just Ignore It? The Domino Effect of Complications
This isn't fearmongering; it's physiology. An untreated dental infection doesn't just sit still.
- Bone Loss: The infection erodes the jawbone around the tooth root, which can complicate future treatments like implants.
- Tooth Loss: The bone loss gets so severe the tooth falls out.
- Spread of Infection: This is the scary part. The infection can spread to your:
- Sinuses: Causing a sinus infection.
- Jaw (Osteomyelitis): A serious bone infection.
- Soft Tissues: Causing cellulitis in your face or neck.
- Bloodstream (Sepsis): A life-threatening systemic infection.
The cost and complexity of treating these complications are astronomically higher than dealing with the original infected tooth. It's simply not worth the gamble.
How to Prevent Infected Teeth in the First Place
Prevention is cheaper, easier, and pain-free. It boils down to a few consistent habits.
- Brush twice a day with fluoride toothpaste. Don't rush it – two full minutes.
- Floss every day. Yes, every day. This cleans the sides your brush can't reach, where gum disease starts.
- Use an antiseptic or fluoride mouthwash if recommended by your dentist.
- Limit sugary and acidic snacks and drinks. They fuel the bacteria that cause decay.
- Drink fluoridated water.
- Don't use your teeth as tools to open packages or crack nuts.
- Wear a mouthguard if you play sports or grind your teeth at night.
And the big one:
These visits catch cavities when they're small and cheap to fix, long before they become painful infected teeth. They also catch early gum disease. It's the best insurance policy you can buy for your mouth.
Common Questions About Infected Teeth (Answered)

Will antibiotics cure my infected tooth?
No. As we covered, they control the spreading infection but don't remove the source. You must follow up with a root canal or extraction.
Can a tooth infection heal on its own?
Almost never. The body can't regrow dead pulp or clear a deep-seated bacterial pocket inside a tooth. The pain may subside if the nerve dies completely, but the infection is still active and damaging bone.
How much does it cost to treat an infected tooth?
It varies wildly by location and procedure. A simple extraction might be a few hundred dollars. A root canal and crown on a molar can cost $1,500-$2,500 or more. Dental insurance can offset some costs. The key is that treating it early (a small filling) costs a fraction of this.
Is it safe to wait a few days?
If you only have mild, intermittent pain, you might be able to schedule a non-emergency appointment. But if you have swelling, fever, or severe throbbing pain, waiting is dangerous. Call a dentist immediately.
Can an infected tooth make you sick overall?
Absolutely. Fatigue, fever, and just feeling "run down" are common. A chronic dental infection is a constant burden on your immune system.
What's the difference between a root canal and an extraction?
The root canal cleans out the infection and saves the tooth shell. An extraction removes the entire tooth, infection and all, leaving a gap. Saving your natural tooth is almost always the better long-term choice for your oral health.
Look, dealing with an infected tooth is stressful and painful. But the path forward is clear: recognize the serious symptoms, manage the pain at home temporarily, and get to a professional. Modern dentistry has incredibly effective ways to eliminate the pain and save your smile. The worst action is inaction. Your future self will thank you for taking care of it.