What You’ll Learn
- The Core Process: It's a Battle and a Wall
- Beyond the Basics: The Key Triggers and Risk Factors
- Different Abscesses, Slightly Different Root Causes
- Signs, Symptoms, and Why You Can't Just "Wait It Out"
- Treatment: Addressing the Root Cause Mechanically
- Prevention: Can You Stop the Root Cause Before It Starts?
- Common Questions People Are Too Embarrassed to Ask
Let's be honest, abscesses are the worst. You've probably felt that tender, swollen, and frankly, angry lump under your skin or maybe in your mouth. It's hot to the touch, throbs with a life of its own, and just screams "infection." But have you ever stopped to wonder what is the root cause of an abscess? It's not just a simple pimple that got out of hand. There's a whole biological drama unfolding under your skin, and the star of the show is usually a tiny, unwelcome guest: bacteria.
Most people think it's just dirt or bad luck. I used to think that too, until a friend had a nasty one that landed them in urgent care. The doctor didn't just lance it and send them home; he actually took a minute to explain the chain of events. It was fascinating, in a gross kind of way. The root cause isn't one single thing—it's a perfect storm of invasion, your body's overzealous defense, and a physical trap. Understanding this isn't just academic; it can help you prevent them and know when to seek serious help.
The Core Process: It's a Battle and a Wall
At its heart, answering what is the root cause of an abscess comes down to a failed negotiation between an invader and your immune system. Here's the step-by-step play-by-play of how an abscess forms from scratch.
This is where things go off the rails in a classic case of friendly fire.
So, to directly answer what is the root cause of an abscess? It's a localized collection of pus caused by a bacterial infection that has been walled off by the body's inflammatory response. The root cause is the combination of pathogenic bacteria and an immune response that ends up creating a contained, high-pressure sac of infectious material.
Beyond the Basics: The Key Triggers and Risk Factors
Knowing the process is one thing, but what actually sets it in motion? Why do some people get them and others don't? The "root cause" often has contributing factors that open the door. It's rarely random.
Here are the major players that answer the deeper question of what causes an abscess in practical, everyday terms.
1. The Bacterial Usual Suspects
Not all bacteria are equal in abscess formation.
Staphylococcus aureus is the heavyweight champion, responsible for most skin and soft tissue abscesses. Its strain MRSA (Methicillin-resistant *Staph. aureus*) is particularly troublesome as it's resistant to common antibiotics.
Streptococcus species are also common culprits.
For dental abscesses, it's often a mix of oral bacteria like Streptococcus viridans and anaerobes (bacteria that thrive without oxygen).
I remember reading a study from the CDC on MRSA that highlighted how community-associated strains often present first as abscesses. It's sobering stuff.
2. The Entry Points: How Bacteria Get In
- Minor Skin Trauma: Cuts, scrapes, insect bites, injection sites (especially in intravenous drug use), surgical incisions. Even vigorous scratching can do it.
- Blocked Glands or Follicles: This is huge. A blocked sweat gland (hidradenitis suppurativa), oil gland, or hair follicle (leading to a boil or carbuncle) creates a perfect, fluid-filled, airless environment for bacteria to multiply. This is why abscesses are common in areas with many hair follicles and sweat glands like the armpits, groin, and buttocks.
- Pre-existing Conditions: A dental cavity that reaches the pulp allows bacteria to infect the root, causing a periapical abscess. A clogged sinus can lead to a sinus abscess. A plugged Bartholin's gland duct leads to a Bartholin's abscess.
- Foreign Material: A splinter, stitch, or other foreign object provides a surface for bacteria to cling to and hide from immune cells.
3. The Body's Weakened Defenses (Host Factors)
This is a big one that doesn't get enough attention. Your immune system's strength is a major variable. Factors that suppress it create a permissive environment for abscess formation:
| Risk Factor Category | Specific Examples | Why It Increases Risk |
|---|---|---|
| Medical Conditions | Diabetes (especially poorly controlled), HIV/AIDS, Cancer, Inflammatory Bowel Disease (Crohn's disease is famous for causing fistulating perianal abscesses) | Chronic high blood sugar impairs white blood cell function. Immune system is compromised. Altered anatomy and immune function. |
| Medications | Corticosteroids (like prednisone), Chemotherapy, Immunosuppressants (for transplants or autoimmune diseases) | Directly suppress the inflammatory and immune response, making it harder to fight initial infection. |
| Lifestyle & Other | Obesity, Poor hygiene, Smoking, Intravenous drug use, Chronic skin conditions (eczema, psoriasis) | Creates skin folds prone to moisture and friction. Introduces bacteria and foreign material. Damages skin barrier and blood flow. |
Different Abscesses, Slightly Different Root Causes
While the core process is the same, location adds unique twists to the story of what is the root cause of an abscess.
Common Abscess Types and Their Specific Triggers
- Skin/Boil (Furuncle): Root cause is almost always a Staph aureus infection of a hair follicle. Friction, tight clothing, and shaving are big triggers.
- Dental (Periapical): Root cause is bacteria from a deep cavity or crack invading the tooth's pulp and spreading to the root tip in the jawbone. It's a direct consequence of untreated tooth decay or trauma.
- Pilonidal Abscess: At the top of the buttock cleft. The root cause is believed to be ingrown hairs combined with friction and pressure, creating a sinus that gets infected. More common in hairy men and people who sit for long periods.
- Peritonsillar Abscess (Quinsy): A complication of tonsillitis. Bacteria spread from the infected tonsil into the surrounding tissue. It's a nasty one that can make swallowing feel impossible.
- Internal Abscesses (e.g., in liver, abdomen, brain): These are more serious. The root cause is often bacteria spreading from another infection site via the bloodstream (seeding), from a nearby infected organ (like appendicitis leading to an appendiceal abscess), or after surgery or trauma.
Signs, Symptoms, and Why You Can't Just "Wait It Out"
Recognizing an abscess early is part of understanding its cause and consequence. The symptoms are literally your body's report on the battle.
The classic signs are the cardinal signs of inflammation, plus one: Pain, Redness, Swelling, Heat, and Loss of Function. The loss of function is key—you can't comfortably sit on a pilonidal abscess, you can't chew on a tooth with a dental abscess. The pain is typically constant and throbbing, worsening as pressure builds.
Why is waiting a bad idea? Because that pyogenic membrane makes antibiotics alone less effective. Drugs have trouble penetrating the wall and the low-oxygen, acidic environment inside. The pressure can cause the abscess to burrow deeper or into new tissue planes (creating a sinus or fistula), or it can rupture internally, spreading infection into the bloodstream—a life-threatening condition called sepsis. The UK's National Health Service (NHS) guidelines are clear: a large or growing abscess usually needs professional drainage.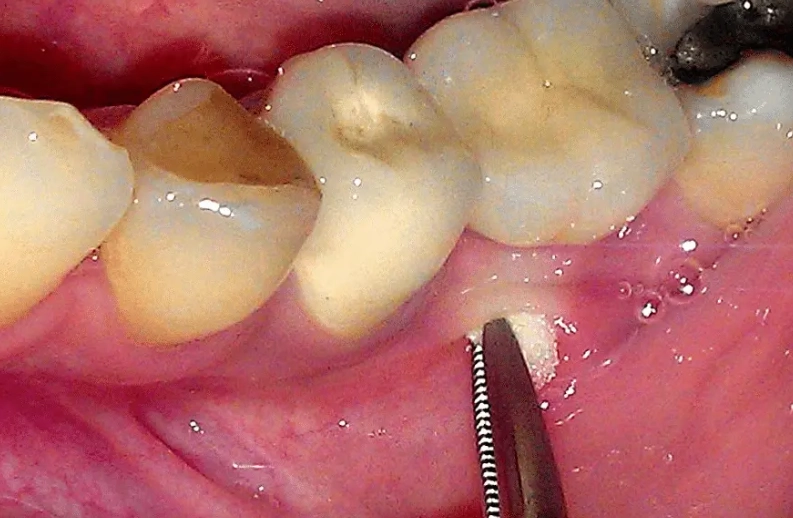
Treatment: Addressing the Root Cause Mechanically
Treatment logically follows from understanding what is the root cause of an abscess. Since the core problem is a walled-off collection of pus under pressure, the primary treatment is to break the wall and relieve the pressure.
- Incision and Drainage (I&D): This is the gold standard for a mature, fluctuant abscess. A healthcare professional makes a cut, lets the pus drain out, and often packs the cavity to keep it open and allow healing from the inside out. The relief is immediate. Antibiotics are often given alongside drainage if the infection is spreading, the person is immunocompromised, or it's in a critical area (like the face).
- Antibiotics: Used for smaller, early-stage infections (cellulitis) to try to prevent abscess formation, or as an adjunct to drainage as mentioned. They target the bacterial root cause but can't dissolve the physical wall of pus.
- Root Canal (for dental abscess): Addresses the root cause directly by removing the infected pulp from inside the tooth, cleaning the canals, and sealing it.
- Warm Compresses: For very small, early boils, applying warmth can increase blood flow and sometimes help the abscess "point" and drain spontaneously on its own. But this is a fine line; if it's not improving in a day or two, see a doctor.
What NOT to Do (The "Home Surgery" Warning)
I feel strongly about this. Do not try to "pop" a deep abscess with a needle, pin, or by squeezing violently. You're likely to push the infection deeper, cause more tissue damage, introduce new bacteria, and create a bigger mess. Leave the lancing to professionals with sterile tools and knowledge of anatomy. Squeezing a facial abscess, in particular, can push bacteria into blood vessels that drain to the brain—a dangerous complication called cavernous sinus thrombosis.
Prevention: Can You Stop the Root Cause Before It Starts?
Knowing what is the root cause of an abscess gives us a blueprint for prevention. It's about protecting the barrier, managing risks, and supporting your immune system.
- Practice Good Wound Care: Clean minor cuts, scrapes, and bites with soap and water. Keep them covered with a clean bandage until healed. It sounds simple, but it's your first line of defense.
- Manage Chronic Conditions: If you have diabetes, work with your doctor to keep your blood sugar well-controlled. This single action dramatically improves white blood cell function.
- Be Mindful of Skin Irritation: Avoid overly tight clothing that causes friction. Be careful when shaving sensitive areas. Keep skin folds clean and dry if you're prone to sweating.
- Don't Share Personal Items: Towels, razors, and washcloths can transfer Staph bacteria.
- Maintain Oral Hygiene: Brush, floss, and see your dentist regularly. A dental abscess is almost entirely preventable with good dental care.
- Support Your Immune System: Eat a balanced diet, get enough sleep, manage stress, and don't smoke. The basics matter.
Common Questions People Are Too Embarrassed to Ask
The pus inside is teeming with bacteria, so yes, the drainage is contagious. If someone has direct contact with the draining pus, they could potentially get the bacteria on their skin and, if they have a break in their skin, develop their own infection. Keep a draining abscess covered with a clean, absorbent dressing and practice good hand hygiene.
Recurrence in the same area is frustrating and points to an unresolved root cause. It could mean the initial abscess wasn't fully drained, a foreign body (like a hair fragment in a pilonidal sinus) remains, or there's an underlying anatomical issue (like a blocked gland) or condition (like hidradenitis suppurativa). You might need a specialist to investigate the deeper cause.
This is a fantastic question that clarifies the process. Cellulitis is a diffuse, spreading infection of the skin and tissues beneath it. It's like the early alarm stage (inflammation) without the walled-off pus collection. An abscess is the later, contained result. Cellulitis can sometimes progress to form an abscess if the infection becomes localized. The treatment differs—cellulitis usually requires oral or IV antibiotics, while an abscess requires drainage.
Not directly. Stress doesn't create bacteria or a break in the skin. However, chronic stress can weaken your immune system over time, making you more susceptible to all kinds of infections, including those that could lead to an abscess. So it's an indirect risk factor, not a root cause.
Figuring out what is the root cause of an abscess takes you from seeing it as a random, painful lump to understanding it as a specific biological event with clear triggers. It's a story of defense gone awry, of a physical barrier becoming a prison for infection. The good news is that this knowledge is power—the power to prevent them when possible, to seek the right treatment promptly, and to demystify a very common, yet poorly understood, health issue. If you suspect you have one, especially if it's large, painful, or accompanied by fever, please see a doctor or dentist. Don't let it simmer; the pressure needs to go.
Leave a Reply