A periapical abscess isn't just a bad toothache. It's a pocket of pus that forms at the very tip of your tooth's root, and it's your body's last-ditch effort to contain an infection that's already won the battle inside your tooth. If you've ever felt a throbbing, persistent pain that seems to come from deep within your jawbone, especially when you bite down, you might be dealing with this. The problem is, many people try to tough it out with painkillers, not realizing the infection is silently eating away at the bone that holds the tooth in place. I've seen patients who waited until their face was swollen to seek help, turning a manageable dental procedure into a complex emergency.
Quick Navigation
What Exactly Is a Periapical Abscess?
Think of your tooth like a house. The hard enamel is the exterior walls. Inside, there's a living space called the pulp chamber, which contains nerves, blood vessels, and connective tissue. This chamber has a long basement that extends down each root—the root canal. When bacteria break through the walls (from a deep cavity or crack), they invade this living space.
The body fights back, sending immune cells. That fight creates pus—a mix of dead tissue, bacteria, and white blood cells. As pressure builds in the confined root canal space, the infection is forced out the tiny opening at the root's tip (the apex), into the jawbone. That's your periapical abscess. "Periapical" literally means "around the apex."
Symptoms You Can't Ignore
The classic sign is a severe, throbbing toothache that doesn't quit. But it's not the only one. People often miss the subtler signals until it's too late.
Here’s a breakdown of symptoms, from the obvious to the easily overlooked:
- Intense, localized pain: A constant, gnawing ache that often worsens when you lie down or apply pressure (chewing).
- Sensitivity to hot and cold: Extreme, lingering pain from temperature changes, especially hot foods/drinks.
- Swelling in the face, cheek, or jaw: This can range from a slight puffiness to a significant, hard swelling that distorts your face.
- Tooth feels "high" or different: The infection can push the tooth slightly out of its socket, making it the first point of contact when you bite.
- Tender, swollen lymph nodes under your jaw or in your neck.
- Fever and general malaise: Your whole body reacts to a significant infection.
- That "pimple on the gum" (fistula): It might drain a bad-tasting, salty fluid, providing temporary relief.
If you have swelling that's making it hard to breathe or swallow, go to an emergency room immediately. That's a sign the infection is spreading to deeper spaces in your neck.
How Does a Tooth Get Infected in the First Place?
The villain is always bacteria. But how do they get all the way to the root tip?
Deep Decay (Cavities)
This is the most common highway. A cavity starts in the enamel, works through the dentin, and finally invades the pulp chamber. Once bacteria are in the pulp, it's game over for the tooth's nerve. The infection travels down the root canals.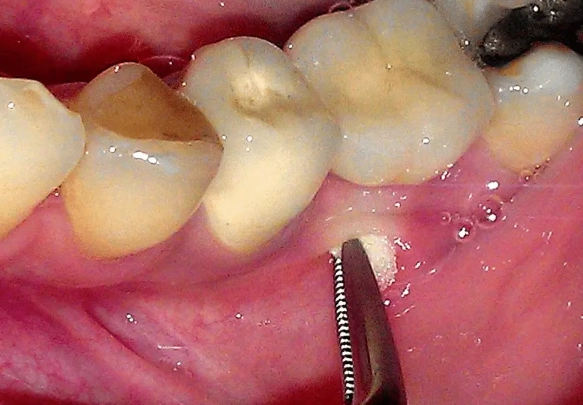
Cracks, Fractures, or Trauma
A hard blow to the tooth, even years ago, can damage the blood supply to the pulp. The tissue slowly dies (necrosis), becoming a sterile playground for bacteria that later find their way in through micro-cracks. A cracked tooth can act as a direct channel for oral bacteria to reach the pulp.
Failed Dental Work
It happens. A deep filling placed close to the pulp can irritate it over time. Or, a previously done root canal might not have fully cleaned one of the intricate, tiny accessory canals, leaving a niche for bacteria to survive and flare up years later.
How Dentists Diagnose a Root Tip Infection
We don't just guess. Diagnosis is a detective game combining your symptoms with clinical tests and imaging.
First, I'll ask about your pain history. Then comes the clinical exam: tapping on teeth (percussion), checking for gum boils, and thermal tests. A key test is the "vitality test," where we apply a cold stimulus. If you feel sharp pain that lingers, or feel nothing at all in a tooth that should feel cold, it's a major red flag for a dead or dying pulp.
The gold standard is the dental X-ray. A periapical radiograph shows the bone around the root tips. A healthy root is surrounded by a thin, uniform black line (the periodontal ligament space). An abscess shows up as a dark, circular shadow at the root's tip—that's the bone loss caused by the infection. Sometimes, in early stages, it won't show on an X-ray. In those cases, a more detailed 3D cone beam CT scan might be needed to see the extent of bone destruction.
Your Treatment Roadmap: Saving the Tooth vs. Removing It
The goal is to eliminate the infection. There are two main paths, and the choice isn't always straightforward.
| Treatment Option | What It Involves | Best For | Key Consideration |
|---|---|---|---|
| Root Canal Treatment (RCT) | Removing infected pulp, cleaning/disinfecting the canal, sealing it, then placing a crown. | Teeth with sound structure above the gumline. | Saves the natural tooth. High long-term success rate (90%+). |
| Tooth Extraction | Removing the entire tooth and root. | Teeth with severe decay/cracks below gum, insufficient bone support. | Immediate cost lower, but creates a gap needing an implant/bridge. |
| Incision & Drainage (I&D) | Making a small cut in the gum to drain pus, relieving pressure. | Emergency measure for severe swelling, done alongside RCT or antibiotics. | Not a standalone cure. Must be followed by definitive treatment. |
| Antibiotics | Oral or IV medication to control spreading infection. | Patients with fever, facial swelling, or compromised immune systems. | Does NOT cure the abscess alone. It's an adjunct to dental treatment. |
Let's talk about the elephant in the room: the root canal. The biggest misconception is that it's a painful procedure. In reality, it stops the pain. The procedure is done under local anesthesia. You'll feel pressure, but not pain. The relief once the infected nerve is removed is almost instant.
The real work happens after. A root-canaled tooth is more brittle and needs a crown to protect it from breaking. Skipping the crown is the number one reason for root canal failure I see—people invest in the procedure but cheap out on the restoration, and the tooth fractures a year later.
What About Cost and Recovery?
A root canal on a molar can cost between $1,000 and $1,800, plus another $1,000-$1,500 for the crown. Extraction is cheaper ($150-$400), but then you're looking at an implant ($3,000-$5,000) or a bridge ($2,000-$5,000). Financially, saving the tooth is often the better long-term investment.
Recovery from a root canal is usually a day or two of mild soreness, manageable with over-the-counter pain relievers. Extraction recovery takes longer, about a week of being careful with the socket.
Can You Prevent a Periapical Abscess?
Absolutely, but it's about consistent, simple habits, not magic.
- Brushing and flossing every day: It's boring, but it removes the plaque biofilm that causes decay. Flossing is non-negotiable for preventing cavities between teeth.
- Regular dental check-ups and cleanings: Every six months. We catch small cavities long before they reach the pulp. A cleaning removes hardened tartar you can't brush away.
- Wear a mouthguard if you play sports or grind your teeth at night (bruxism). Trauma prevention is key.
- Don't ignore tooth pain or sensitivity. That twinge when you eat ice cream? Get it checked. A small filling now prevents a root canal later.
It's that simple, and that hard. Most abscesses I treat are the result of neglected, preventable decay.
Common Questions Answered

1. Destroy so much jawbone that the tooth becomes loose and unsavable.
2. Spread to your sinuses (sinusitis), under your tongue (Ludwig's angina), or into your bloodstream (sepsis), which is life-threatening.
3. Create a cyst in the jaw that requires surgical removal.
I had a patient who ignored a "gum pimple" for a year. The infection eroded through his jawbone and required a bone graft and lengthy surgery. The initial $1,500 root canal turned into a $10,000+ reconstructive nightmare.
The bottom line? A periapical abscess is a serious dental infection that demands professional attention. Pain is your body's alarm system. Don't just silence the alarm—fix the fire. If you suspect you have one, call your dentist. The sooner you address it, the simpler, cheaper, and more successful the treatment will be.
Leave a Reply